Sadhguru: People have no energy because of mental diarrhea. You eat bad food and then try to stop diarrhea, it’s not going to work. This much you do. Tonight, before you go to bed, keep it down and go to bed. In a little while, if you simply sit here, things around you will reverberate. Is it possible to do it without using specific mudras, whatever? Yes. These are all small help, little assistance. You don’t see a Shiva or a Krishna holding mudra and sitting like this, (Gestures) simply intense. Nor will you ever see me sitting like this. (Gestures) No. You will not see me practicing Shambhavi or this or that. If I just close my eyes for 20 seconds, I’m done. I am ready for the day. So, these are all… This is all good help. But is it the only way to do it? No. You can simply sit. If you learn to simply sit, you’ll become tremendously intense. Right now, your energy is simply expended by doing unnecessary endless activities. When you have so much mental diarrhea, how can you have energy? Suppose you have diarrhea, do you see how weak you feel? (Laughter) Yes, or no? Right now, this mental diarrhea, that’s why people have no energy. They want to just eat and sleep all the time because of mental diarrhea, it’s very exhausting. (Laughs) If you have physical diarrhea, you know how exhausting it is. Yes? This is also equally exhausting. People are sleeping eight hours – ten hours a day not because they are working so much or because their body is in such a bad state. It’s just mental diarrhea. If you stop the mental diarrhea, there’s enough energy to make this (Referring to oneself) very, very intense. Now “How do I stop mental diarrhea?” If you have diarrhea… physical diarrhea, what is the first thing to do? Hmm? What? Participants: (Unclear) Sadhguru: Yes, run to the toilet, I know that. (Laughter) I am saying (Laughs) as a corrective measure, what is the first thing you do? No, as a corrective measure, what is the first thing you do? The first thing is to stop eating, right? Yes or no? Diarrhea means in some way we’ve eaten something that the body doesn’t want. It’s trying to throw it out. Yes? You have taken something inside that the body doesn’t like. It wants to throw it out. The first thing is to stay away from food for some time. You eat bad food and then try to stop diarrhea, it’s not going to work. Similarly, bad food for the mind is just this. You have gotten identified with things that you are not. The moment you get identified with things that you are not, mental diarrhea is inevitable. It’s bad food for the mind – now it will run endlessly, do what you want. You do any damn meditation, you say, Shiva, Rama, it’s not going to stop. (Laughs) It’s not stopped, isn’t it? Because bad food is being eaten.

Every day you’re getting identified with more and more things and you want to stop your mind. You do whatever kind of circus, it is not going to stop. If you disidentify with everything – if you understand “what is you” and “what is not you,” if you keep a little distance from that, your mind will become still. If you want you can use it, otherwise you can keep it. Now my hand is there, if I want I can move it, otherwise I can keep it. This is a useful hand. Suppose it starts jumping like this, (Gestures) you clearly know there is some kind of an ailment, isn’t it? Yes or no? So if the hand is jumping, you know it’s an ailment. If the mind is jumping, is it an ailment or not? Participant: Yes. Sadhguru: Ahh. The ailment has come because of a continuous wrong diet. You tell your mind, that “I am this, I am this, I am that, I am that,” it’s having diarrhea. You stop giving it the wrong food. If you clearly see, what… Even if you do not know “what is me,” at least you know “what is not me,” isn’t it? This much you do. Tonight, before you go to bed, sit on your bed and sit down and discount everything that is not you. This house in which you are living, is this me? No. This loving parent or mother, father, wife or husband or child, they are wonderful, but is this me? No. Now these nice clothes I am wearing, is this me? No. Now my body, I like it but is this me? No. Now I’m having so many thoughts, is this me? No. Now I am having wonderful emotions, is this me? No. Like this, everything that’s not you, before you sleep, keep it down and go to bed. Tomorrow morning, you will wake up considerably more intense than today. Every day you do it. In a little while, if you simply sit here, things around you will reverberate, really. A few years ago… a couple of years ago I was in America and this is a very typical American question – this lady (Laughs) comes up to me and she’s very angry. “I have been doing this yoga for the last 35 years, nothing happened. But you went and just sat on a rock and things happened to you. (Laughter) This is not fair. Where is that damn rock?” (Laughter) She thinks it’s the rock that did it. (Laughter) The only sadhana that I did in my life is, right from a very early age, though I was very actively involved with everybody around me, I never identified myself with my parents or my siblings or my endless number of friends or the society or the religion or the country or anything around me – never identified, not that I was not involved. I was very involved and very active. Even today I am very active and involved but not identified. If you don’t identify with anything, there is enough energy in this (Referring to oneself) to become intense. See I want you to understand, your life energy right now in this body, how many things it’s doing here as you’re sitting here! Hello, do you know the complexity of the activity it is doing? Every cell in the body, your liver, your kidney, your damn spleen, and all kinds of stupid things that we cannot even figure even today, yes? Just see as you sit here, how many things this energy is doing. Obviously, it must be intense to do all this. You are not able to experience it because of diarrhea. (Few laugh) Tch… When you have diarrhea, (Gestures) that’s how you feel, isn’t it? Yes or no? So that’s how it is. Stop the diarrhea, stop eating bad food, diarrhea will stop. Once the diarrhea stops, there’s enough energy in this to sit here and reverberate in a very intense way.
As found on YouTube15 Modules Of Intimate Video Training With
Dr. Joe Vitale – You’re getting simple and proven steps to unlock the Awakened Millionaire Mindset: giving you a path to MORE money, …

 At this point, Tom knows a lot about himself
but doesn’t connect well with others. To him, people seem to follow rules
without questioning them— just like sheep. Integrating into the society is difficult at
this point and he begins to search for utopia. Mira makes it into a top medical school where she
realizes, she’ll never be top of the class again. Once that place seems out of reach,
her motivation drops and she wonders if medicine interests
her. Since quitting is no option, she takes up a second major and
runs for student council president. Soon Mira will know everything about what
others expect, but nothing about what she likes for herself. All her life she has just
listened – driven by external feedback loops. At this point, she’s also lost the ability to
question the norms of the society she grew up in. Listening to our hearts can tell us who we
are, but not how to be happy among others. Listening to others can motivate us to be
a part of their world, but doesn’t teach us if that world is ours. This is why it’s
probably good for the two to go together. Then we can learn what we want, and
get the feedback that we need to stay motivated to explore
new roads into a better society. A large body of research shows that balancing
the two forces is not straightforward. One meta-analysis of 128 studies examined the effects
of extrinsic rewards on intrinsic motivation. While most rewards significantly
undermine our intrinsic interest, positive feedback — which is an extrinsic
motivator — inspires us to keep going. Put simply, honest words of
encouragement get us going, while money or gifts undermine our inner drive. What about you? Do you listen to your
heart or the voices of society? And from your personal experience, which
of the two eventually takes your decision? Share your thoughts and check the
description to dive deeper into the topic. Sprouts videos are published under the Creative
Commons License. That means our videos are free and anyone can download, edit, and play them for
personal use. Public schools, governments, and non-profit organizations can also use them
for training, online courses, or designing new curriculums. To help us stay independent and
support our work, you can join our patrons and contribute. Just visit patreon.com/sprouts.
Even one dollar can make a difference.As found on YouTubeExplaindio Agency Edition FREE Training How to Create Explainer Videos & SELL or RENT them! Join this FREE webinar | Work Less & Earn More With Explaindio AGENCY EDITION
At this point, Tom knows a lot about himself
but doesn’t connect well with others. To him, people seem to follow rules
without questioning them— just like sheep. Integrating into the society is difficult at
this point and he begins to search for utopia. Mira makes it into a top medical school where she
realizes, she’ll never be top of the class again. Once that place seems out of reach,
her motivation drops and she wonders if medicine interests
her. Since quitting is no option, she takes up a second major and
runs for student council president. Soon Mira will know everything about what
others expect, but nothing about what she likes for herself. All her life she has just
listened – driven by external feedback loops. At this point, she’s also lost the ability to
question the norms of the society she grew up in. Listening to our hearts can tell us who we
are, but not how to be happy among others. Listening to others can motivate us to be
a part of their world, but doesn’t teach us if that world is ours. This is why it’s
probably good for the two to go together. Then we can learn what we want, and
get the feedback that we need to stay motivated to explore
new roads into a better society. A large body of research shows that balancing
the two forces is not straightforward. One meta-analysis of 128 studies examined the effects
of extrinsic rewards on intrinsic motivation. While most rewards significantly
undermine our intrinsic interest, positive feedback — which is an extrinsic
motivator — inspires us to keep going. Put simply, honest words of
encouragement get us going, while money or gifts undermine our inner drive. What about you? Do you listen to your
heart or the voices of society? And from your personal experience, which
of the two eventually takes your decision? Share your thoughts and check the
description to dive deeper into the topic. Sprouts videos are published under the Creative
Commons License. That means our videos are free and anyone can download, edit, and play them for
personal use. Public schools, governments, and non-profit organizations can also use them
for training, online courses, or designing new curriculums. To help us stay independent and
support our work, you can join our patrons and contribute. Just visit patreon.com/sprouts.
Even one dollar can make a difference.As found on YouTubeExplaindio Agency Edition FREE Training How to Create Explainer Videos & SELL or RENT them! Join this FREE webinar | Work Less & Earn More With Explaindio AGENCY EDITION
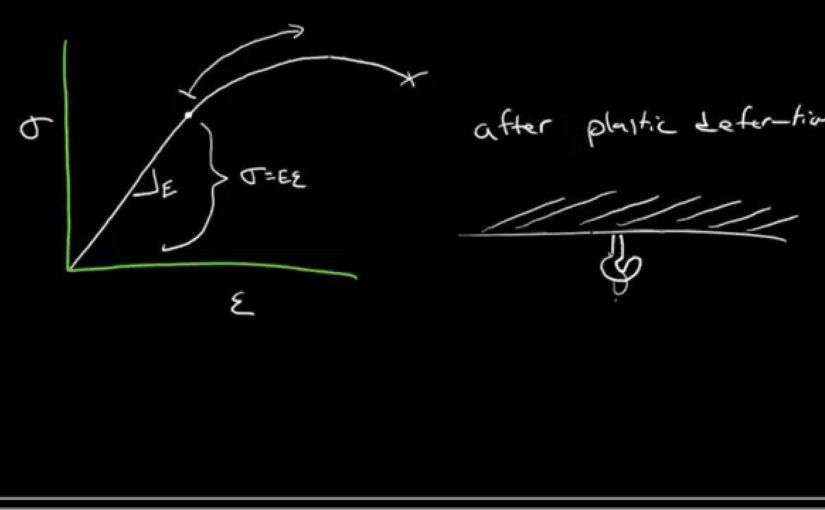
 And so if you do that
for infinitely small– infinitesimally small
changes in length, the way we would write that
is we’d have to say, the true strain, what we’re
doing is we’re integrating. We’re integrating those
infinitesimally small changes in length– that’s dl– by l
from l0– the initial length– to the instantaneous length. And so if we do that,
you find that you have ln of l instantaneous
minus length 0, which is ln of l instantaneous over l0. So we have another
equation there. I’ll put a box around that. So this is the true strain. True strain. And if we take that true
stress and we plot it against the true strain,
I’ll show you what we get. Let me just
plot stress and strain and I’ll show you what
we’ve already seen. That’s the engineering
stress-strain curve. And then what I’ll do is I’ll
plot for you– after it starts to plastically deform the–
ran out of space there– the true stress– so this one
here– continues to increase. It doesn’t have that
decrease at the UTS. That’s the true stress
true strain curve. And this one is, of
course, engineering. The nice thing
about this plot is once you’ve got true
stress and true strain, we can fit that data
quite nicely for most metals with a simple equation. And that is true stress
is equal to this coefficient times the true strain
raised to the power n. So that’s an equation that fits
that true stress true strain data quite nicely. And what’s useful about
this is these are constants. That’s the constant n– I’ll
define it for you in a moment– and this K is also a constant. Those are material properties. We can look those up in
an engineering handbook. So n is called the–
well, this equation is called the
strain-hardening equation. Strain hardening equation. And strain hardening– hardening
correlates to– hardness correlates to strength. So really this is
the equation that’s telling us that we’re
strengthening the material and we’ve got the
strain hardening exponent and the strain
hardening coefficient K.
And so if you do that
for infinitely small– infinitesimally small
changes in length, the way we would write that
is we’d have to say, the true strain, what we’re
doing is we’re integrating. We’re integrating those
infinitesimally small changes in length– that’s dl– by l
from l0– the initial length– to the instantaneous length. And so if we do that,
you find that you have ln of l instantaneous
minus length 0, which is ln of l instantaneous over l0. So we have another
equation there. I’ll put a box around that. So this is the true strain. True strain. And if we take that true
stress and we plot it against the true strain,
I’ll show you what we get. Let me just
plot stress and strain and I’ll show you what
we’ve already seen. That’s the engineering
stress-strain curve. And then what I’ll do is I’ll
plot for you– after it starts to plastically deform the–
ran out of space there– the true stress– so this one
here– continues to increase. It doesn’t have that
decrease at the UTS. That’s the true stress
true strain curve. And this one is, of
course, engineering. The nice thing
about this plot is once you’ve got true
stress and true strain, we can fit that data
quite nicely for most metals with a simple equation. And that is true stress
is equal to this coefficient times the true strain
raised to the power n. So that’s an equation that fits
that true stress true strain data quite nicely. And what’s useful about
this is these are constants. That’s the constant n– I’ll
define it for you in a moment– and this K is also a constant. Those are material properties. We can look those up in
an engineering handbook. So n is called the–
well, this equation is called the
strain-hardening equation. Strain hardening equation. And strain hardening– hardening
correlates to– hardness correlates to strength. So really this is
the equation that’s telling us that we’re
strengthening the material and we’ve got the
strain hardening exponent and the strain
hardening coefficient K.
 Every day you’re getting identified with more and more things and you want to stop your mind. You do whatever kind of circus, it is not going to stop. If you disidentify with everything – if you understand “what is you” and “what is not you,” if you keep a little distance from that, your mind will become still. If you want you can use it, otherwise you can keep it. Now my hand is there, if I want I can move it, otherwise I can keep it. This is a useful hand. Suppose it starts jumping like this, (Gestures) you clearly know there is some kind of an ailment, isn’t it? Yes or no? So if the hand is jumping, you know it’s an ailment. If the mind is jumping, is it an ailment or not? Participant: Yes. Sadhguru: Ahh. The ailment has come because of a continuous wrong diet. You tell your mind, that “I am this, I am this, I am that, I am that,” it’s having diarrhea. You stop giving it the wrong food. If you clearly see, what… Even if you do not know “what is me,” at least you know “what is not me,” isn’t it? This much you do. Tonight, before you go to bed, sit on your bed and sit down and discount everything that is not you. This house in which you are living, is this me? No. This loving parent or mother, father, wife or husband or child, they are wonderful, but is this me? No. Now these nice clothes I am wearing, is this me? No. Now my body, I like it but is this me? No. Now I’m having so many thoughts, is this me? No. Now I am having wonderful emotions, is this me? No. Like this, everything that’s not you, before you sleep, keep it down and go to bed. Tomorrow morning, you will wake up considerably more intense than today. Every day you do it. In a little while, if you simply sit here, things around you will reverberate, really. A few years ago… a couple of years ago I was in America and this is a very typical American question – this lady (Laughs) comes up to me and she’s very angry. “I have been doing this yoga for the last 35 years, nothing happened. But you went and just sat on a rock and things happened to you. (Laughter) This is not fair. Where is that damn rock?” (Laughter) She thinks it’s the rock that did it. (Laughter) The only sadhana that I did in my life is, right from a very early age, though I was very actively involved with everybody around me, I never identified myself with my parents or my siblings or my endless number of friends or the society or the religion or the country or anything around me – never identified, not that I was not involved. I was very involved and very active. Even today I am very active and involved but not identified. If you don’t identify with anything, there is enough energy in this (Referring to oneself) to become intense. See I want you to understand, your life energy right now in this body, how many things it’s doing here as you’re sitting here! Hello, do you know the complexity of the activity it is doing? Every cell in the body, your liver, your kidney, your damn spleen, and all kinds of stupid things that we cannot even figure even today, yes? Just see as you sit here, how many things this energy is doing. Obviously, it must be intense to do all this. You are not able to experience it because of diarrhea. (Few laugh) Tch… When you have diarrhea, (Gestures) that’s how you feel, isn’t it? Yes or no? So that’s how it is. Stop the diarrhea, stop eating bad food, diarrhea will stop. Once the diarrhea stops, there’s enough energy in this to sit here and reverberate in a very intense way.
Every day you’re getting identified with more and more things and you want to stop your mind. You do whatever kind of circus, it is not going to stop. If you disidentify with everything – if you understand “what is you” and “what is not you,” if you keep a little distance from that, your mind will become still. If you want you can use it, otherwise you can keep it. Now my hand is there, if I want I can move it, otherwise I can keep it. This is a useful hand. Suppose it starts jumping like this, (Gestures) you clearly know there is some kind of an ailment, isn’t it? Yes or no? So if the hand is jumping, you know it’s an ailment. If the mind is jumping, is it an ailment or not? Participant: Yes. Sadhguru: Ahh. The ailment has come because of a continuous wrong diet. You tell your mind, that “I am this, I am this, I am that, I am that,” it’s having diarrhea. You stop giving it the wrong food. If you clearly see, what… Even if you do not know “what is me,” at least you know “what is not me,” isn’t it? This much you do. Tonight, before you go to bed, sit on your bed and sit down and discount everything that is not you. This house in which you are living, is this me? No. This loving parent or mother, father, wife or husband or child, they are wonderful, but is this me? No. Now these nice clothes I am wearing, is this me? No. Now my body, I like it but is this me? No. Now I’m having so many thoughts, is this me? No. Now I am having wonderful emotions, is this me? No. Like this, everything that’s not you, before you sleep, keep it down and go to bed. Tomorrow morning, you will wake up considerably more intense than today. Every day you do it. In a little while, if you simply sit here, things around you will reverberate, really. A few years ago… a couple of years ago I was in America and this is a very typical American question – this lady (Laughs) comes up to me and she’s very angry. “I have been doing this yoga for the last 35 years, nothing happened. But you went and just sat on a rock and things happened to you. (Laughter) This is not fair. Where is that damn rock?” (Laughter) She thinks it’s the rock that did it. (Laughter) The only sadhana that I did in my life is, right from a very early age, though I was very actively involved with everybody around me, I never identified myself with my parents or my siblings or my endless number of friends or the society or the religion or the country or anything around me – never identified, not that I was not involved. I was very involved and very active. Even today I am very active and involved but not identified. If you don’t identify with anything, there is enough energy in this (Referring to oneself) to become intense. See I want you to understand, your life energy right now in this body, how many things it’s doing here as you’re sitting here! Hello, do you know the complexity of the activity it is doing? Every cell in the body, your liver, your kidney, your damn spleen, and all kinds of stupid things that we cannot even figure even today, yes? Just see as you sit here, how many things this energy is doing. Obviously, it must be intense to do all this. You are not able to experience it because of diarrhea. (Few laugh) Tch… When you have diarrhea, (Gestures) that’s how you feel, isn’t it? Yes or no? So that’s how it is. Stop the diarrhea, stop eating bad food, diarrhea will stop. Once the diarrhea stops, there’s enough energy in this to sit here and reverberate in a very intense way.



 Do Something You Enjoy If you’re feeling stressed, take some time off to relax your mind and body Watch. Your favorite TV show listen to music, go for a walk, do anything you want. Try daily meditation breaks to release a small amount of stress. The point is to relax. You can also find some campus resources that can help. You manage your stress like the University Counseling Center. They offer consultations in Spanish or English and it’s always confidential. They also provide workshops on how to deal with stress. All their services are free for students enrolled at UTEP. Everyone experiences levels of stress, however, when you realize it you can take charge. Take your mind off things and relax plan and organize your time wisely Manage your stress before it manages you.
Do Something You Enjoy If you’re feeling stressed, take some time off to relax your mind and body Watch. Your favorite TV show listen to music, go for a walk, do anything you want. Try daily meditation breaks to release a small amount of stress. The point is to relax. You can also find some campus resources that can help. You manage your stress like the University Counseling Center. They offer consultations in Spanish or English and it’s always confidential. They also provide workshops on how to deal with stress. All their services are free for students enrolled at UTEP. Everyone experiences levels of stress, however, when you realize it you can take charge. Take your mind off things and relax plan and organize your time wisely Manage your stress before it manages you.
 This article was authored by Adnan Alzahrani Chris Keyworth, Caitlin, Wilson, and others.
This article was authored by Adnan Alzahrani Chris Keyworth, Caitlin, Wilson, and others.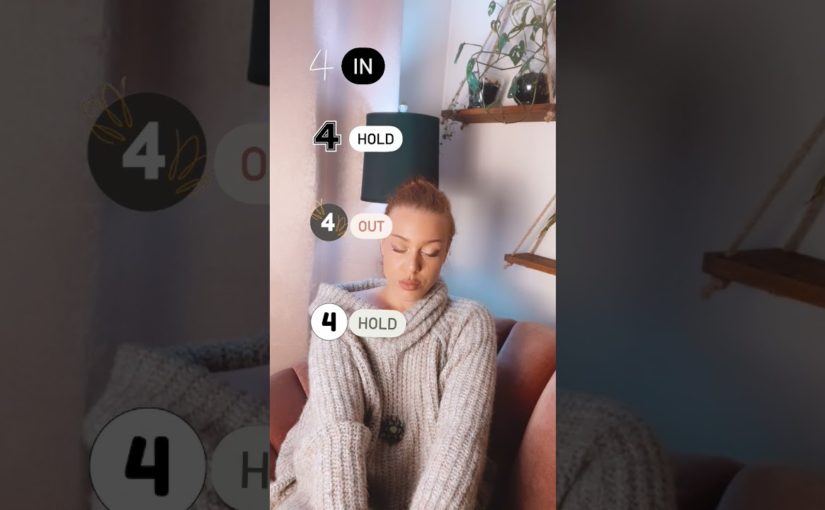
 3. 4 Hold 2, 3, 4, Now exhale, 2, 3, 4 And hold 2 3 4 Excellent. We can try something new next time and I’ll see you then, please note you can adapt this count to whatever feels most comfortable to you. Bye.
3. 4 Hold 2, 3, 4, Now exhale, 2, 3, 4 And hold 2 3 4 Excellent. We can try something new next time and I’ll see you then, please note you can adapt this count to whatever feels most comfortable to you. Bye.

 Number four, not feeling pain. Another sign of dissociation
is not feeling pain. There is research suggesting that dissociation not only
minimizes painful memories but also the physical
pain attached to them. However, the connection
between dissociation and pain is not solely related to trauma. People who experience chronic pain can also experience dissociation. For some who experience dissociation as a result of a mental health condition, the feeling of not feeling in your body can sometimes lead you to self-injure. Although it makes sense to do something to bring you back into your body, self-injuring is not the best option. And number five, a loss of self-identity. Another aspect of dissociation
is depersonalization, it’s similar to derealization in the sense that you feel like you
are watching yourself. However, depersonalization
makes you feel distant from your mental process, you feel that you are an
observer of your own life. Depersonalization can
occur with other symptoms on this list, it can be a very scary feeling like you don’t have any
control of your body. Some clinicians believe that
extreme stress or trauma can produce depersonalization. So, do you relate to any of these signs? Dissociation can be frightening and, in some cases, intrusive. It’s not like a physical illness where a diagnosis and treatment are administered via exams, but there is treatment, among them being
psychotherapy, medication, family therapy, and clinical hypnosis. If you experience any of these symptoms, please reach out to a medical health
professional for treatment. Please like and share this with friends who might find some good
advice in the video as well. Make sure to subscribe to Psych2Go and hit the notification
bell for more content. All the references used are added in the description box below. Thanks so very much for watching and we’ll see you the next time.My Name Is Dr. Joe Vitale
Number four, not feeling pain. Another sign of dissociation
is not feeling pain. There is research suggesting that dissociation not only
minimizes painful memories but also the physical
pain attached to them. However, the connection
between dissociation and pain is not solely related to trauma. People who experience chronic pain can also experience dissociation. For some who experience dissociation as a result of a mental health condition, the feeling of not feeling in your body can sometimes lead you to self-injure. Although it makes sense to do something to bring you back into your body, self-injuring is not the best option. And number five, a loss of self-identity. Another aspect of dissociation
is depersonalization, it’s similar to derealization in the sense that you feel like you
are watching yourself. However, depersonalization
makes you feel distant from your mental process, you feel that you are an
observer of your own life. Depersonalization can
occur with other symptoms on this list, it can be a very scary feeling like you don’t have any
control of your body. Some clinicians believe that
extreme stress or trauma can produce depersonalization. So, do you relate to any of these signs? Dissociation can be frightening and, in some cases, intrusive. It’s not like a physical illness where a diagnosis and treatment are administered via exams, but there is treatment, among them being
psychotherapy, medication, family therapy, and clinical hypnosis. If you experience any of these symptoms, please reach out to a medical health
professional for treatment. Please like and share this with friends who might find some good
advice in the video as well. Make sure to subscribe to Psych2Go and hit the notification
bell for more content. All the references used are added in the description box below. Thanks so very much for watching and we’ll see you the next time.My Name Is Dr. Joe Vitale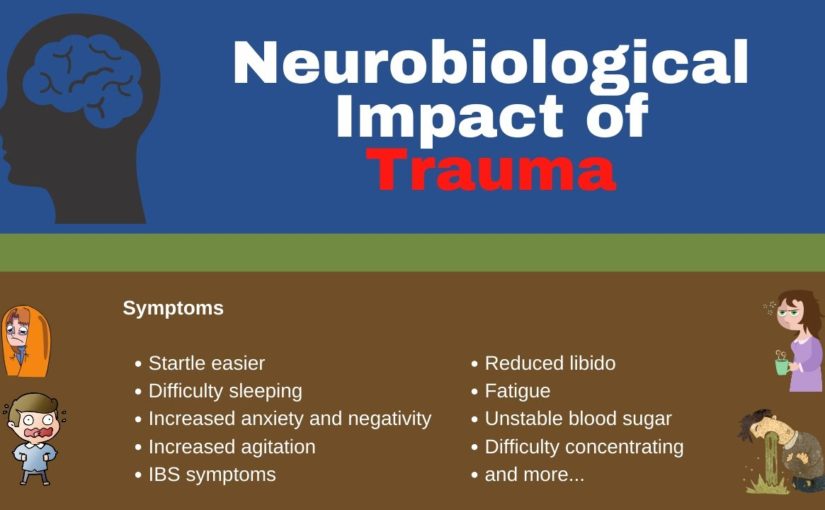
 Which means the brain’s
ability to adjust and adapt as well as learning and memory so these are good receptors I like
them glutamate binds with these receptors and high levels of glutamate are secreted during high
levels of stress glutamate remember is what GABA is made from but high levels of glutamate
it’s an excitatory neural net in the brain and overexposure of neurons to this glutamate can be
excited toxic and may contribute to the loss of neurons in the hippocampus of patients with PTSD
so we’re actually seeing brain volume decrease as a result of exposure to certain chemicals elevated
gluten core glucocorticoid and yeah glucocorticoids increases the sensitivity of these receptors so
you’ve got a bunch of glutamate being dumped and you’ve got a bunch of glucocorticoid you’ve got
cortisol in there making these receptors more sensitive so it’s got they’re more sensitive and
they’ve got more coming in which makes it a whole lot easier to become toxic and start causing
neuronal degradation what does that mean why do we care it may take clients with PTSD more time to
master new skills because of emotional reactivity but also because some of their synaptic plasticity
may be damaged so it may take them a little bit longer to actually acquire and integrate these
new skills it’s not saying they’re stupid they can remember it just fine however when they’re
an emotionally charged state and helping their brain learn that okay this isn’t a threat that’s one
of those sort of subconscious things that has to happen that can take longer if the brain becomes
excited toxic during stress inhibited learning and memory then it becomes excited toxic during
stress which inhibits learning and memory so it’s under stress things are excited toxic neurons
are starting to disappear so I’m wondering and I’m just hypothesizing here I don’t know the
answers obviously or I wouldn’t be practicing it but what happens during the exposure therapies
because that’s exactly what we’re doing is we are flooding the brain with all of these chemicals
and creating basically an excitotoxin now they found some evidence that exposure therapies can
be helpful according to the DOJ website but or not the DOJ I can’t even think of it right
now the VA website but you know I’m wondering long-term what the impact is endogenous opioids
natural painkillers act upon the same receptors activated by exogenous opioids like morphine and
heroin exerts an inhibitory influence on the HPA axis well we know that people take opiates
and it has depressant effects on them it slows them down and calms them down alterations in our
natural opioids may be involved in certain PTSD symptoms such as numbing stress-induced analgesia
and dissociation again think of any clients you’ve had who have been abused or even taken and not like
the side effects of opiates are what opiates do to some people make them feel more relaxed stress
induced and analgesia they don’t have as much physical pain sometimes they just it’s there
I don’t care pill another interesting factor is now truck zone which is used to oppose opiate
appears to be effective in treating symptoms of dissociation flashbacks in traumatized persons so
basically, they’re saying if we undo the endogenous opioids we can treat these symptoms it highlights
the risk of opiate abuse for persons with PTSD though because if endogenous opioids produce
some of these numbing symptoms and dissociative symptoms so they can get away from the pain and
the flashbacks then if they add to that you know oral opioids it could prove to be a very tempting
cocktail we do want to as clinicians figure out how we can assist them with their physical and
emotional distress tolerance so they don’t feel the need to numb and escape and you know I
can’t imagine what some people have seen have gone through and I’m not trying to take that away
from them, I’m trying to help them figure out how they can stay present and learn to integrate it
changes question marks in brain structure and one of the questions that’s come up in the research is
because there aren’t any longitudinal studies that looked at it was the hippocampal volume as low to
begin with which created a predisposition for PTSD or did PTSD create the smaller hippocampal volume
interesting hippocampus is implicated in the control of stress responses memory and contextual
aspects of fear conditioning so it helps you to find these triggers in the environment that
help you become aware with your senses about when there might be a trauma prolonged exposure
to stress and high levels of glucocorticoids damage the hippocampus we’ve talked about that
hippocampal volume reduction in PTSD may reflect the accumulated toxic effects of repeated exposure
to increased cortisol levels what I called earlier the flatter the Furious having you know your body
holding on to cortisol for this extreme stress and then when it perceives stress it’s either
nothing or it’s extreme there are no kind sort of mild stressors out there that decrease hippocampal
volumes might also be a pre-existing vulnerability factor for developing PTSD the amygdala yet
another brain structure is the Olympic structure involved in the emotional process and it’s
critical for the acquisition of fear responses functional imaging of studies has revealed hyper
responsiveness and PTSD during the presentation of stressful script cues or trauma reminders but
also patients show increased amygdala responses to general emotional stimuli that are not trauma
associated such as emotional faces so they show an increased responsivity to things they see on the
TV that aren’t trauma-related to people crying to people showing anger’s going to have a
stronger emotional amygdala response than people without PTSD so clients with PTSD may be more
emotionally responsive across the board leading to more emotional dysregulation again an area that
we can help provide them with tools for early adverse experiences including prenatal stress and stress
throughout childhood has profound and long-lasting effects on the development of neurobiological
symptoms the brain is developing and if is exposed to a lot of stress and some of these excited toxic
situations how does that differ in the amount of damage caused versus a brain that’s already kind
of pretty much-formed programming may change for subsequent stress reactivity and vulnerability
to develop PTSD so if these happen during childhood or at any time the brain can
basically reprogram and go that it’s a really dangerous place out there so I need to hold
on to cortisol and I need to hold on to these stress hormones because every time I turn around
it seems like there’s a threat so I am going to be hyper-vigilant and respond in an exaggerated way
to protect you from the outside world adult women with childhood trauma histories have been shown
to exhibit sensitization of both neuroendocrine and Audino stress responses so basically they’re
showing hypo cortisol ISM a variety of changes take place in the brains and nervous systems of
people with PTSD and we talked about a lot of those the key take-home point is stress can
actually get toxic in the brain and cause physical changes not just thought changes in the brain
preexisting issues causing hypo cortisol ism where the brain has already downregulated whether it’s
due to chronic illness or chronic psychological stress increases the likelihood of the development
of PTSD this points to the importance of prevention and early intervention of adverse
childhood experiences we really need to get in there and help these people develop distress
tolerance skills understanding of vulnerabilities so they’re not going from flat to furious all
the time and so that they can understand why their body kind of responds and why they respond
differently than others and you know as we talk about this and of course I’m regularly bringing up
DBT buzzwords if you will think about your clients if you’ve worked with any who’ve had borderline
personality disorder what kind of history do they have did they have just a great childhood no we
know that people with BPD generally had pretty chaotic childhoods so this research is also
kind of underscoring why they may react and act the way they do that flat to furious people with
hypo cortical ism may or may not have PTSD so we don’t want to say well you’re fine if you don’t
have PTSD symptoms we do know that every trauma potentially can cause the body to down-regulate
and I kind of look at it as conserving a little bit more of the energy that it needs each time so
instead of conserving 60% now it’s conserving 65 and 66 each time it encounters a stressor in order
to prepare for potential ongoing threats in the environment hypercortisolism sets the stage for
the flattened the furious leading to toxic levels of glutamate upon exposure to stressors which
can cause the theorized reduction in hippocampal volume and persistent negative brain changes now I
always say the brain can you know rebalance itself and all well that’s part of the plasticity that is
the really cool thing about our brain however as far as regenerating those neurons I haven’t found
any evidence in the research that we found a way to help people regenerate once we’ve already those
neurons are gone they’ve been killed off the brain has to find a workaround so it does take time
but I do believe people can minimize some of the impact of the trauma they may have experienced
people with PTSD are more reactive to emotional stimuli even stimuli unrelated to trauma again
think about some of your clients especially if you work in a residential situation where you’re
around on 24/7, you know for 30 or 60 days, and you may see some clients that seem to get upset
over everything and you’re like ah such a drama queen or such a drama king and to yourself not
to anybody else but when you think about it from this perspective it gives you a different
perspective and you might say oh maybe their body responds differently they’ve got more emotional
dysregulation because of prior trauma they’re not trying to overreact this is their body’s response
because it’s perceived threat so many times it gives me a different approach to working
with that client hypercortisolism results when the brain perceives that continued effort is futile
feelings of fatigue set in akin to reduced stress tolerance so think about you know when you’ve had
a really long stressful period you know weeks or months maybe you’re dealing with an ailing family
member or something it’s just a lot of stress and you start getting really tired and when you’re
really tired and you’re worn down and somebody gives you one more thing it’s that one more thing
normally wouldn’t bother you but right now you just can’t take it so we can see how there’s a
reduced stress tolerance when somebody’s already at this stage reducing fatigue in our clients can
be accomplished in part with psychological factors including motivation or knowledge of other people
who are dealing with similar things support groups feedback about their and making sure they have
frequent successes not once a week but I want to have them keep a journal every day of something
good that happened or something positive that may indicate they’re moving forward in their
treatment goals and knowledge of an endpoint.
Which means the brain’s
ability to adjust and adapt as well as learning and memory so these are good receptors I like
them glutamate binds with these receptors and high levels of glutamate are secreted during high
levels of stress glutamate remember is what GABA is made from but high levels of glutamate
it’s an excitatory neural net in the brain and overexposure of neurons to this glutamate can be
excited toxic and may contribute to the loss of neurons in the hippocampus of patients with PTSD
so we’re actually seeing brain volume decrease as a result of exposure to certain chemicals elevated
gluten core glucocorticoid and yeah glucocorticoids increases the sensitivity of these receptors so
you’ve got a bunch of glutamate being dumped and you’ve got a bunch of glucocorticoid you’ve got
cortisol in there making these receptors more sensitive so it’s got they’re more sensitive and
they’ve got more coming in which makes it a whole lot easier to become toxic and start causing
neuronal degradation what does that mean why do we care it may take clients with PTSD more time to
master new skills because of emotional reactivity but also because some of their synaptic plasticity
may be damaged so it may take them a little bit longer to actually acquire and integrate these
new skills it’s not saying they’re stupid they can remember it just fine however when they’re
an emotionally charged state and helping their brain learn that okay this isn’t a threat that’s one
of those sort of subconscious things that has to happen that can take longer if the brain becomes
excited toxic during stress inhibited learning and memory then it becomes excited toxic during
stress which inhibits learning and memory so it’s under stress things are excited toxic neurons
are starting to disappear so I’m wondering and I’m just hypothesizing here I don’t know the
answers obviously or I wouldn’t be practicing it but what happens during the exposure therapies
because that’s exactly what we’re doing is we are flooding the brain with all of these chemicals
and creating basically an excitotoxin now they found some evidence that exposure therapies can
be helpful according to the DOJ website but or not the DOJ I can’t even think of it right
now the VA website but you know I’m wondering long-term what the impact is endogenous opioids
natural painkillers act upon the same receptors activated by exogenous opioids like morphine and
heroin exerts an inhibitory influence on the HPA axis well we know that people take opiates
and it has depressant effects on them it slows them down and calms them down alterations in our
natural opioids may be involved in certain PTSD symptoms such as numbing stress-induced analgesia
and dissociation again think of any clients you’ve had who have been abused or even taken and not like
the side effects of opiates are what opiates do to some people make them feel more relaxed stress
induced and analgesia they don’t have as much physical pain sometimes they just it’s there
I don’t care pill another interesting factor is now truck zone which is used to oppose opiate
appears to be effective in treating symptoms of dissociation flashbacks in traumatized persons so
basically, they’re saying if we undo the endogenous opioids we can treat these symptoms it highlights
the risk of opiate abuse for persons with PTSD though because if endogenous opioids produce
some of these numbing symptoms and dissociative symptoms so they can get away from the pain and
the flashbacks then if they add to that you know oral opioids it could prove to be a very tempting
cocktail we do want to as clinicians figure out how we can assist them with their physical and
emotional distress tolerance so they don’t feel the need to numb and escape and you know I
can’t imagine what some people have seen have gone through and I’m not trying to take that away
from them, I’m trying to help them figure out how they can stay present and learn to integrate it
changes question marks in brain structure and one of the questions that’s come up in the research is
because there aren’t any longitudinal studies that looked at it was the hippocampal volume as low to
begin with which created a predisposition for PTSD or did PTSD create the smaller hippocampal volume
interesting hippocampus is implicated in the control of stress responses memory and contextual
aspects of fear conditioning so it helps you to find these triggers in the environment that
help you become aware with your senses about when there might be a trauma prolonged exposure
to stress and high levels of glucocorticoids damage the hippocampus we’ve talked about that
hippocampal volume reduction in PTSD may reflect the accumulated toxic effects of repeated exposure
to increased cortisol levels what I called earlier the flatter the Furious having you know your body
holding on to cortisol for this extreme stress and then when it perceives stress it’s either
nothing or it’s extreme there are no kind sort of mild stressors out there that decrease hippocampal
volumes might also be a pre-existing vulnerability factor for developing PTSD the amygdala yet
another brain structure is the Olympic structure involved in the emotional process and it’s
critical for the acquisition of fear responses functional imaging of studies has revealed hyper
responsiveness and PTSD during the presentation of stressful script cues or trauma reminders but
also patients show increased amygdala responses to general emotional stimuli that are not trauma
associated such as emotional faces so they show an increased responsivity to things they see on the
TV that aren’t trauma-related to people crying to people showing anger’s going to have a
stronger emotional amygdala response than people without PTSD so clients with PTSD may be more
emotionally responsive across the board leading to more emotional dysregulation again an area that
we can help provide them with tools for early adverse experiences including prenatal stress and stress
throughout childhood has profound and long-lasting effects on the development of neurobiological
symptoms the brain is developing and if is exposed to a lot of stress and some of these excited toxic
situations how does that differ in the amount of damage caused versus a brain that’s already kind
of pretty much-formed programming may change for subsequent stress reactivity and vulnerability
to develop PTSD so if these happen during childhood or at any time the brain can
basically reprogram and go that it’s a really dangerous place out there so I need to hold
on to cortisol and I need to hold on to these stress hormones because every time I turn around
it seems like there’s a threat so I am going to be hyper-vigilant and respond in an exaggerated way
to protect you from the outside world adult women with childhood trauma histories have been shown
to exhibit sensitization of both neuroendocrine and Audino stress responses so basically they’re
showing hypo cortisol ISM a variety of changes take place in the brains and nervous systems of
people with PTSD and we talked about a lot of those the key take-home point is stress can
actually get toxic in the brain and cause physical changes not just thought changes in the brain
preexisting issues causing hypo cortisol ism where the brain has already downregulated whether it’s
due to chronic illness or chronic psychological stress increases the likelihood of the development
of PTSD this points to the importance of prevention and early intervention of adverse
childhood experiences we really need to get in there and help these people develop distress
tolerance skills understanding of vulnerabilities so they’re not going from flat to furious all
the time and so that they can understand why their body kind of responds and why they respond
differently than others and you know as we talk about this and of course I’m regularly bringing up
DBT buzzwords if you will think about your clients if you’ve worked with any who’ve had borderline
personality disorder what kind of history do they have did they have just a great childhood no we
know that people with BPD generally had pretty chaotic childhoods so this research is also
kind of underscoring why they may react and act the way they do that flat to furious people with
hypo cortical ism may or may not have PTSD so we don’t want to say well you’re fine if you don’t
have PTSD symptoms we do know that every trauma potentially can cause the body to down-regulate
and I kind of look at it as conserving a little bit more of the energy that it needs each time so
instead of conserving 60% now it’s conserving 65 and 66 each time it encounters a stressor in order
to prepare for potential ongoing threats in the environment hypercortisolism sets the stage for
the flattened the furious leading to toxic levels of glutamate upon exposure to stressors which
can cause the theorized reduction in hippocampal volume and persistent negative brain changes now I
always say the brain can you know rebalance itself and all well that’s part of the plasticity that is
the really cool thing about our brain however as far as regenerating those neurons I haven’t found
any evidence in the research that we found a way to help people regenerate once we’ve already those
neurons are gone they’ve been killed off the brain has to find a workaround so it does take time
but I do believe people can minimize some of the impact of the trauma they may have experienced
people with PTSD are more reactive to emotional stimuli even stimuli unrelated to trauma again
think about some of your clients especially if you work in a residential situation where you’re
around on 24/7, you know for 30 or 60 days, and you may see some clients that seem to get upset
over everything and you’re like ah such a drama queen or such a drama king and to yourself not
to anybody else but when you think about it from this perspective it gives you a different
perspective and you might say oh maybe their body responds differently they’ve got more emotional
dysregulation because of prior trauma they’re not trying to overreact this is their body’s response
because it’s perceived threat so many times it gives me a different approach to working
with that client hypercortisolism results when the brain perceives that continued effort is futile
feelings of fatigue set in akin to reduced stress tolerance so think about you know when you’ve had
a really long stressful period you know weeks or months maybe you’re dealing with an ailing family
member or something it’s just a lot of stress and you start getting really tired and when you’re
really tired and you’re worn down and somebody gives you one more thing it’s that one more thing
normally wouldn’t bother you but right now you just can’t take it so we can see how there’s a
reduced stress tolerance when somebody’s already at this stage reducing fatigue in our clients can
be accomplished in part with psychological factors including motivation or knowledge of other people
who are dealing with similar things support groups feedback about their and making sure they have
frequent successes not once a week but I want to have them keep a journal every day of something
good that happened or something positive that may indicate they’re moving forward in their
treatment goals and knowledge of an endpoint.