this episode was pre-recorded
as part of a live continuing education webinar on-demand CEUs are
still available for this presentation AllCEUs.com/Anxiety-CEU I’d like to welcome everybody to today’s
presentation on best practices for the treatment of anxiety I am your host, Dr. Dawn Elise Snipes now not too long ago we did
a presentation on strengths-based biopsychosocial approaches to addressing anxiety while
those are wonderful you know I thought maybe we ought to look at you know what’s some of the
current research so I went into PubMed which is I don’t know it’s a playground for me it’s where
you find a lot of journal articles and you can sort I sorted by articles that were
done and meta-analyses that were done within the past five years so that gives us an idea
about current research I mean there’s a lot of stuff that is still the same like some of
the medications that were known to work ten years ago are still known to be you know good
first-line treatments but there are also some newcomers that we’ll talk about and there are
also some changes that we’re going to talk about so we’re going to explore some common causes
for anxiety symptoms to treat, we need to and of course, this does play into
the biopsychosocial aspect we need to understand kind of what causes it because anxiety
that’s caused by for example somebody having a racing heart may be different than anxiety that’s
caused for somebody who has abandonment issues so we’re gonna treat the two things differently so
we want to look at some of the common causes we’re gonna look at some common triggers for anxiety
Do you know what are some of these common themes that we see in practice I will ask you to share
some of the themes that you see that underline or underlie a lot of your client’s anxiety and
identify current best practices for anxiety management including counseling interventions
medications physical interventions and supportive treatments so we care because anxiety can
be debilitating and a lot of our clients have anxiety a lot of our clients have anxiety
comorbid with depression and they’re looking at us going how can I feel anxious and stressed out
and like I can’t sit still and be depressed at the same time you know when you’re depressed you’re
supposed to want to sleep well a lot of times people who have both issues want to
sleep but they can’t so I want to help clients understand that also sometimes anxiety when
people are anxious for long enough the body starts kind of holding on to the cortisol the body
recognizes at a certain point this is a losing battle I’m not going to put energy into
this anymore so it starts withdrawing some of its excitatory neurotransmitters so to speak and
people will start to feel depressed the brain has already said this is hopeless this is
you’re helpless to change the situation so then people start feeling hopeless and helpless
which is sort of the definition if you will of depression low-grade chronic stress and anxiety
arose energy and people’s ability to concentrate so if we’re going to help them become their uber
selves we need to help them figure out how to address anxiety not just generalized overwhelming
debilitating anxiety but also panic social anxiety and those minor anxiety triggers that come along
that may not meet the threshold for diagnosis anxiety is a major trigger for addiction relapse
if you have a client who is self-medicated before or had an addiction for some reason anxiety is a
major trigger increased physical pain when anxiety goes up people tend to tense their muscles when
they tense their muscles they tend to feel more pain I mean think about when you’re stressed you
tend to have more pain like in your neck your back and things that already hurt may hurt more
why because serotonin which is one of our major anti-anxiety neurotransmitters is also one of our
major pain modulators so when serotonin levels are too low because anxiety is high then our pain
perception is going to be more acute and people can have sleep problems if they’re stressed out
your body thinks there’s a threat you’re not going to be able to get into that deep restful
sleep you may have you may sleep you may sleep a lot but it’s probably not quality sleep which
means your neurotransmitters may get out of whack your hormones make it out of whack and your body
is going to start perceiving yourself in a persistent state of stress when you’re exhausted
the body knows that we may be the weakest link in the herd so it continues to secrete cortisol
to keep you on alert a little bit so you may again you may be resting kind of like when
you have a new baby at home those first couple of months that my children were home from the
hospital I slept but I didn’t sleep well I mean the slightest little noise and I was awake and I
was looking around and you know I felt it I felt exhausted and a lot of new parents do so triggers
for anxiety abandonment and rejection and we’re going to talk about ways we might want to deal
with these things but some of the underlying themes that I’ve seen in a lot of clients and when
I do the research and a lot of what themes that come out include low self-esteem if someone has
low self-esteem they’re looking to be externally validated oftentimes they’re looking for somebody
else to tell them you’re lovable you’re okay so that can lead to anxiety about not having
people to tell them you’re okay which makes their relationships tenuous and can make them
dysfunctional irrational thoughts and cognitive distortions may lead people to believe that if I’m
not perfect for example I am not lovable so we’re going to look at some irrational thoughts and
cognitive distortions unhealthy social supports and relationships when you’re in a relationship
it takes two to tango and even if your client is relatively mentally and physically healthy if they
are in a dysfunctional relationship they can fear abandonment and rejection if that other person
is always saying if you don’t do X I’m going to leave you or if that other person is always
cheating on them or whatever so relationships can trigger abandonment anxiety and ineffective
interpersonal skills can lead to relationship turmoil and social exile if our clients are in
relationships even if they’re not completely dysfunctional if our clients are not able to ask
for what they need and set appropriate boundaries and manage conflict effectively because conflict
happens in every relationship then they may start to argue more which may lead to fearing may lead
to relationships ending in the past and them going well every relationship I get into ends which
means I must not be lovable so they start fearing abandonment and rejection these are four areas
that we can look at one more assessing clients another issue is the unknown and loss of control
a lot of times negative self-talk and cognitive distortions can contribute to that if I don’t have
control of everything then it’s all going to be a disaster negative others when clients hang out
or when people hang out with negative people it kind of wears on you after a while you notice
that people who tend to be more negative pessimistic conspiracy-minded tend to hang out
with people who are also negatively pessimistic and conspiracy-minded so if you’re hanging out with
somebody who tends to be anxious then the anxiety can be palpable and it can kind of permeate
physical complaints can lead people to be anxious because they don’t know what’s causing it
like I said earlier sometimes if your heart starts to race if you don’t know what’s causing it you
can start thinking I’m having a heart attack or I’m gonna die when people have panic attacks for
the example they truly think they’re having a heart attack and it’s I’ve had them they are very
very unpleasant experiences but when people start having physical complaints and it can be you
know they have a weird rash that they can’t get to go away or whatever but when they don’t know
what it is and they can’t control it they can’t make it go away they start thinking about all
the worst-case scenarios and going online and getting on WebMD which usually gives you all the
worst-case scenarios um so physical complaints are important we need to normalize the fact that
nobody’s pain-free all the time and you know the fact that you may have an ache or a pain or a lump
or a bump or you know a cough most likely you know when we look at probability the probability of it
being something significant is pretty small now do you want to get it checked out probably but
you know the probability that is anything to be worried about is relatively small and a sense
of powerlessness can trigger fear of the unknown and loss of control for somebody who doesn’t
feel like they have any agency in their life if they have an external locus of control or
if they felt victimized all of their life then they may fear not being in control they may be
holding on and saying okay this is the one area of my life I can control when I grew up you know
I grew up in a very chaotic environment I had no control I was bounced around in the foster system
yadda yadda yadda now that I’m an adult you know I can control these things and I am going to hold
on with white knuckles and if I can’t control everything then that terrifies me to death and
loss are other triggers for anxiety and it can be people or pets and pets are important I don’t
want to minimize pets because you know they are little parts of a lot of our families so making
sure we check that my daughter’s dog for example is it’s getting old she’s getting older she’s 14
now I think and you know she’s in decent health we took her to the vet and the vet said yeah she’s
got a little heart murmur but that’s expected for a 14-year-old dog and but when she goes out if she
doesn’t come back when I call her I have this rush of anxiety for a second oh my gosh I hope this
wasn’t the day so anxious around losing people and you know if she when she crosses the bridge
she will and you know I’m okay with that I’m I have a harder time dealing with my daughter’s
emotional turmoil when that happens and because she’s grown up with this dog so you know those
are the types of things that we want to talk about with our clients what things are weighing on you
that you may not even be thinking about because I know in the back of my mind there’s always that
worry about one of our donkeys and her dog jobs and promotions can trigger anxiety if people are
afraid they’re gonna lose their job if they’re always afraid that you know they’re gonna walk in
and get a pink slip or get fired you know we want to help them look at how realistic they are
you doing what you need to do to achieve and keep your job and sometimes it’s not easy to
answer I mean the first thought that a lot of us have is well you know if you’re doing the right
thing so just do it but there are those bosses out there and I’ve had some amazing bosses
a lot of them and I’ve had two horrendous bosses and those two bosses I could never I
never felt like I was able to do anything right and so going to those jobs there was always this
anxiety about what I’m what am I going to get in trouble for today so you want to talk with people
about does your job cause anxiety what can you do to moderate that anxiety the same thing with
promotions people may get anxious about whether they’re going to get promoted to safety and security
you know when you lose safety and security you can feel anxious so if there’s a break-in at
the house next door or shooting down the road or you start watching the news you can feel very
unsafe and insecure quickly so we want to help people figure out how safe and secure are you
really and a lot of it goes back to really looking at facts when people lose their dreams and hopes
or fear that they’re going to lose their dreams and hopes they can start to get anxious you know
they have this dream that they’re going to be a doctor or I just finished the presentation on
helping high school students transition to college and a lot of high school students for example
start college with these wide eyes and hopes to save the world and they want to be doctors
and engineers and this and that and they get into it and they realize that it’s a lot harder
then they thought or they realize that you know what I don’t like this but I’ve already
committed to it so what do I do I want to help people but I can’t I can’t cut it doing this you
know for me I figured out in my second year that I wasn’t going to medical school because I wasn’t
going to pass calculus and that caused a lot of anxiety it was like okay what am I gonna do now
Do you know what career should I choose to help people figure out do they have dreams that have
maybe kind of crashed and burned and you have to find new ones you know okay that one we’ve got to
accept it figure out that it’s not going to be and what can you do now people may also have dreams
about relationships, they get into relationships and see themselves with this person forever
and then this relationship ends and or starts to get rocky and they’re like but that’s my dream
what happens if that’s got to happen because it’s my dream I don’t know how to function if
that goes away we want to help people be able to rewrite their narrative and then sickness spiders
and other phobias kind of go in with death a lot of times when people get sick they start getting
anxious that oh my gosh what if this is terminal oh my gosh what if this is you know incurable
if I get bit by a spider it’s gonna kill me and which is rare you know there are very few spiders
that is that poisonous same thing with snakes going over bridges I’ve shared with you all
that is not one of my irrational fears you know I am just terrified that you know something’s going
to happen and I’m going to get pushed off the side of the bridge which is completely irrational but
we need to help people look at those and identify the thoughts that they’re telling themself about
those phobias and dealing with that anxiety failure is another trigger for anxiety especially in
this culture our culture American culture is in large part puts a high premium on success
and perfectionism so when people realize that they’re not perfect they may start to get anxious
because they feel like if I’m not perfect then I’m a failure you know those cognitive distortions of
all-or-nothing thinking and they start with that negative self-talk you know you can’t do anything
right so those are some of the issues that you know we often see in counseling sessions so what
do we do you know somebody comes in and is like I can’t live this way doc anxiety depression and
substance disorders as well as a range of physical disorders are often comorbid so this is the first
the thing we need to realize is that we’re very rarely dealing with a very simple
diagnosis you know when somebody comes in we need to figure out you know if they come in and they’re
presenting with depression all right let’s talk about that and then we start realizing that there
depression started to occur after a long period of being anxious okay so we need
to deal with that but we also need to help them with their sense of hopelessness and helplessness
we need to develop that sense of empowerment and then substance disorders we know that substance
use is often a way of self-medicating but we also know that it monkeys with the neurochemicals
in the brain and can contribute to anxiety and depression the same thing to physical issues pain
from physical disorders anxiety about having physical disorders medications you’re taking for
physical disorders can all contribute to anxiety so we need to look at the person as a whole and go
what are all the things that are contributing to the anxiety and what are all the things that the
anxiety is contributing to so we have started having this big list of stuff that needs to be
addressed and then we can start figuring out okay where we start so knowing that these things
are comorbid helps researchers explore pathways to mental disorders so they can start figuring
out you know what little string can we pull to unravel this blanket of anxiety so it doesn’t
suffocate somebody and for us as clinicians it provides us key opportunities to intervene in you
know sometimes clients will come in and start talking about their
anxiety and their physical issues you know maybe their anxieties about you know heart
palpitations and because that’s a common one we may want to encourage them to go see the doctor to
get that ruled out you know rule out anything that has to do with hormone imbalances or you know
heart conditions or anything else that might be contributing to it which can help them address
it and if they do have physical disorders let’s go with hormone imbalances that are contributing
to the heart palpitations then they can start to treat that if they don’t start to treat that then
no amount of talk therapy we do is going to get them to the quality of life that they’re looking
for because they’re still gonna feel those so we want to make sure that we’re addressing them
holistically anxiety disorders should be treated with psychological therapy pharmacy therapy or a
combination of both and what they found and this is no surprise this is kind of old news is that
counseling Plus pharmacotherapy tends to have the best outcomes but separating the two have
similar outcomes in many cases but that’s just looking at and I hate to call it simple anxiety
but we’re just looking at anxiety symptoms here we’re not looking at the full quality of life and we
want to make sure that we’re also including any medical issues behavioral therapy is regarded
as the psychotherapy with the highest level of evidence, there are a variety of cognitive
behavioral approaches ranging from acceptance and commitment therapy to dialectical behavior
therapy to CBT to debt you know any of those that deal with the thoughts and the cognitions that fall in
that realm and it is effective in the current conceptualization of the etiology
of anxiety disorders includes an interaction of psychosocial factors such as childhood adversity
or stressful events and a genetic vulnerability so the psychosocial factors and these are other
things when we do our assessment we want to pay attention to because our approach to treatment
is going to be different for people for example who have trauma-related brain changes maybe
then for somebody who doesn’t so, we want to look at childhood adversity and stressful events
that it may have caused basically what I tell clients is like rewiring of the brain there
are trauma-related brain changes in soldiers and especially in children or in people who’ve been
exposed to extreme trauma that is designed to protect them but it also can cause complications
kind of later on in dealing with anxiety coping skills that were learned that are ineffective you
know sometimes people grow up in a household or an environment or a situation where they don’t learn
effective coping skills so we need to kind of help them unlearn those and learn new ones build on
their strengths and trauma issues that may still need to be dealt with such as domestic violence
you know if they grew up a lot around a lot of domestic violence they may think you know I’m
out of that situation it’s over I don’t want to think about it it’s not bothering me anymore or a
parental absence and I put absence because it can be death it can be a parent that just packed up
and left it could be a child that got put up for adoption whatever put the child in a position of
feeling like they were rejected by a parent can be very traumatic and bullying among other things
but there are a lot of trauma issues that people once they’re out of that situation often say you
know I’m out of it it’s not a big deal I dealt with it let’s move on and they don’t realize the
full ramifications and how that’s contributing to their current anxiety and their current self-talk
and cognitions of current stressors if somebody has a lot of current stressors that’s also going to
impact whether they develop generalized anxiety you know we’re kind of stacking the deck here and
the current availability of social support if they don’t have effective current social support then
they’re gonna have difficulty bearing the weight of everything on their shoulders so we want
to look at all these psychosocial factors when we do our assessment now going back to the trauma
issues if you’ve taken the trauma courses at all CEUs you know that some people are not ready
to acknowledge that the trauma is still bothering them or work on the trauma and that’s okay we
can educate them that it might be an issue and then let them choose how to address it but
we want to bear in mind the fact that you know this could be sort of an underlying force
motivating some of the current cognitions and genetic vulnerability so you take any three
people and you put them or 300 people and you put them through roughly the same psychosocial
situations they’re all probably going to react a little bit differently based on their prior
experiences but also because of their genetic makeup there are certain permutations and they
found four we’ll talk about later that make the brain more or less responsive to stress and
more or less responsive to serotonin which is your calming chemical so brains that are less
responsive to serotonin isn’t going to you know send out as much or send out serotonin as easily
so people can stay kind of tensed and wired that’s an oversimplified explanation but that’s
all you need for right now so genetic vulnerability impacts people’s susceptibility
to the effects and development of dependence on certain substances which can increase anxiety
when people are detoxing from alcohol when they’re detoxing from benzos when they’re detoxing from
opiates they can feel high levels of anxiety when they take opiates some people find that opiates
have wonderful anti-anxiety properties not that I am advocating for the use of opiates I’m
just client experiences have shown that that can be true so some people are going to be
more susceptible to the anti-anxiety effects of certain substances and some people are going
to be Cerrone to become dependent on substances where others may not and that part of that is
genetic vulnerability and they estimate about 30% the predictability of the development
of anxiety disorders is genetic and genetics also impact which medications are effective
if you have genetic makeup then SSRIs might be helpful then
atypical antipsychotics may be more effective and SSRIs might not do anything which is why
a lot of our clients get so frustrated because they know there’s no way to figure out exactly what I
guess there is now that there’s genetic testing out there but up until then it was harder to
figure out which medications to start with and most physicians matter of fact I don’t know of
a single physician that starts by saying well let’s do a genetic profile to see
what med to start you out with most we’ll start with events as with an SSRI or some other
anti-anxiety medication some sort of Benzo that’s been my experience so we may want
to encourage clients to consider genetic testing if they’re having difficulty finding a
medication regime that works for them and they are feeling like they have to have medication
genetic vulnerability also affects what’s going to make somebody more vulnerable now than all of you
in class today you know thinking about sleep you know sleep may not be a big deal for some of you
I know people who can go days or weeks with four or five hours of sleep and they feel fine it’s
not a big deal, not me I need eight or nine hours of sleep so genetically for whatever reason I am
programmed to need a lot of sleep so when I don’t get that much sleep I tend to be it tends to be
harder for me to deal with life on life’s terms and I know that that makes me more vulnerable to
being irritable so genetic vulnerability affects who can become addicted and affects what medications
work best and affects what situations are going to tend to make somebody more vulnerable to
anxiety so our medications and I know the type on here is small but we’re going to go through
the first-line drugs are the SSRIs selective serotonin reuptake inhibitors and SNRs is
selective norepinephrine reuptake inhibitors now the names are a little bit deceptive because
selective norepinephrine reuptake inhibitors also increase available serotonin but the mechanism
of action is different the mechanism of action for each SSRI is a little bit different as well
which is why you can put somebody on Prozac and they have an awful experience and you can put them
on Zoloft and they have a much better experience like I said earlier a lot of the research pre
five years ago had been done on medications and Zoloft paxil luvox lexapro celexa and their
generics have all been found to be effective at treating anxiety in certain people no one
medication works for everybody in the last five years effexor has come on the radar and it has
been found effective according to the Hamilton rating scale for anxiety so that’s another one to
consider if clients are not successful or getting the treatment effect that they need for on some
of the other medications obviously, none of us probably are prescribers but we do need to educate
clients about why the first drug or even the third drug that the doc tries may not work so they
don’t start feeling helpless and hopeless like I said earlier there are at least four different
genetic variations which are correlated with the development of generalized anxiety disorder and
different medications are more or less effective depending on the genetic makeup of the person
there’s a high mortality rate moving on to two benzos the recommendation has switched
to back off from the use of benzos now for some doctors will prescribe an SSRI and for the
first, four weeks while the SSRI is building up in the system they will also prescribe a Benzo
to be taken as needed to moderate the anxiety and you know you could argue on either side
of that, if somebody has a history of substance use or substance dependence benzos are really
a bad idea because they do have a high rate of dependence but the other reasons that they are now
cautioning against the use of benzodiazepines is that there’s a higher mortality rate among benzo
users compared with non-users there’s an increased risk for dependence with use for more than six
months and that’s a long time to be using Benzo and when we’re talking about dependence and six
months we’re talking about somebody who uses it like every four hours or every eight hours
depending on your Benzo every single day, not a PRN user if somebody’s using it at night to
help them go to sleep or you know three or four times a week when the anxiety gets high
the risk of dependence is relatively low but a lot of people with anxiety because if they find
the right Benzo makes them feel so much better they may not want to be off of it and for a lot of
people when that benzo reaches its half-life and starts getting out of the system even more their
anxiety spikes you know they have rebound anxiety which they want to medicate with more benzos
that’s gonna be an issue for them to discuss with their doctor there’s also an increased risk
of dementia identified in long-term benzodiazepine users again this is for the people who use you
know throughout the day every day for six months or relatively every day for six months or more
and it doesn’t matter if it’s you know we’re talking about somebody who’s 65 or somebody
who’s 35 who’s been using Benzos for you know six months a year two years the risk of later
life dementia is greatly increased according to the research benzodiazepines also don’t treat
depression okay so if you’ve got somebody who has concurrent anxiety and depression there’s a much
higher suicide risk if they’re on benzodiazepines so being aware and generally that suicide risk
comes from overdosing on benzodiazepines but not always other treatment options you know if the
benzos aren’t something that people want to touch you know they scare the living daylights out of
I SSRIs and SNRIs don’t seem to be working then tricyclic antidepressants can be tried on those
your older generation antidepressant seroquel is used a lot and there are some there’s some
research that shows it can be effective with anxiety like some of the antidepressants and
depending on the person the benzos seroquel can make people very very very sleepy so you know
it may not be the side effects of the Seroquel the weight gain and the fatigue and you know
sleepiness may be an unacceptable side effect for some clients and boosts perón is the third option
boost Barone works more like an anti-depressive serotonin reuptake inhibitor and that it takes
you know four weeks or so to kind of build up in the system studies have shown that there’s really
no long-term benefit to taking it but after six months to eighteen months of use it has been shown to
be effective in talking with clients a lot of clients report that boost bar when they take it
doesn’t necessarily help them stop being anxious like a benzodiazepine does but it helps them not
go from zero to 200 in 2.3 seconds it kind of you know keeps them from having this gush of a freak
out reaction every time something goes wrong which a lot of clients report helps because they feel
more stable throughout the day after remission medication should be continued for six to twelve
months and during that last six months first six months keep it as is last six months you know
they say that tapering is best it’s best not to stop somebody cold turkey on any of these but
it’s important for people once they’re in remission to not just suddenly go okay I feel
better I don’t need any of this anymore they need to work into it and make sure they’ve developed
the skills and tools that they need to deal with some of the anxiety that is going to
happen in life so physical signs and symptoms of anxiety may include fatigue irritability muscle
tension or muscle aches try laying feeling twitchy being easily startled trouble sleeping nausea
diarrhea irritable bowel syndrome headaches so the first thing we want to do with clients when we’re
talking to them well second thing first thing is say get a physical let’s rule out physiological
causes of this but we can also help clients look at you know what might be causing these
things that you can do to mitigate it what might be contributing to your fatigue what might be
contributing to your irritability and your muscle tension or your muscle aches I mean let’s look at
economics did you recently get a new bed or do you need to get a new bed what about your desk chair I
know you know I get more muscle tension and muscle achy when I do a lot of mousing because I have
deplorable posture being becoming aware of that helps and then I’m like okay well I know it caused
unfortunately, it’s unpleasant but it’s not a big deal trembling or feeling twitchy you know
that can be caused by low blood sugar that can be caused anxiety that can also be caused
by early onset Parkinson’s symptoms you know there’s you know it can be worst case scenario
or it can be something benign so we want to have people figure out you know when you start
trembling or feeling twitchy is there something that it’s related to you know I know when my
son gets excited he’s he just sits there and you can see him almost shake because he’s so
excited about something so we want to have people prevent misidentification we don’t want them
to jump to that worst-case scenario we don’t want them to go onto WebMD and go oh my gosh I’ve
got cancer I’ve got this debilitating disease and I’m going to die in six months probabilistic Lee
speaking it’s not gonna happen yes get a doctor’s opinion I’m certainly not going to tell them it’s
all in your head I want them to get an evaluation but I do want to in the meantime
help them think about how likely is this and other things for headaches and this is
one another one of those that can be frustrating as we get older our eyesight starts to go and
you know there was a period there I did fine and then after I hit 45 my eyesight just started
to like steadily and kind of rapidly in my mind decline so I have to get my eyeglass prescription
changed every couple of years and that can cause headaches so instead of starting to worry
about oh my gosh I’ve got a headache all the time maybe I’ve got a brain tumor you know I know that
it’s probably my glasses or I’m grinding my teeth so other biological interventions that
have been evaluated there’s something called the floatation rest system that reduced environmental
stimulation therapy reduces sensory input into the nervous system through the act of floating
supine which is on your back in a pool of water saturated with Epsom salt you know I’m looking at
this going sounds good and you can’t quite get the same experience in a bathtub because
you’re not floating you’ve got pressure points and you’re still hearing stuff clients can sort of
simulate it with you know earplugs or whatever but it’s if they can access this it’s been shown
to be effective the float experience is calibrated so that sensory signals from visual
auditory olfactory gustatory thermal tactile or tactile vestibular gravitational and preceptive
channels are minimized which means you don’t see here taste touch smell feel anything as is most
movement and speech so you want people to lay just like completely motionless and not talk which can
be hard for some people with anxiety in the study the study I looked at fifty participants
reported significant reductions in stress muscle tension pain depression and negative effects and it
was accompanied by significant improvement in mood characterized by increases in relaxation happiness
and well-being I read the study I’m like where can I sign up you know it sounds in looking at some of
the research this was more effective for addressing anxiety than something like a massage
Tai Chi also produced significant reductions in anxiety there was approximately a 20% treatment
effect 25% treatment effect in patients with anxiety and fibromyalgia who practiced twice a
week for a year now you know we want to look at the confounding things here is it the Tai Chi
itself or is it learning to control the muscles and becoming more in tune with your body and
learning to control your breathing helps people reduce their anxiety either way you know
Tai Chi helps people do that and it was shown that after a year after the first six months, there was
a significant treatment effect but after a year you know it kept growing and after a year it was
about 25% so Tai Chi can be effective acupuncture at the HT 7 median Meridian can
attenuate anxiety-like behavior induced by withdrawal from chronic morphine treatment through
the meditation of the GABA receptor system what does that mean that means if you if the
acupuncture is done in very certain places the anxiety behavior the GABA a receptor
system GABA is your main calming relaxation neurochemical that is triggered and causes your
body to sort of flood that receptor system and this research was done on people who were detoxing
from morphine treatment but we can look at generalizing the results and I would be interested
to see further studies on it pain other things we need to do to help people with anxiety when people
are in chronic pain they often have anxiety that oh my gosh this is getting worse or It’s never
gonna get better or I just can’t take this pain anymore or they may get anxious that they’re going
to be rejected because they can’t do some of the things they used to do because they’re in so much
pain so there’s a lot of guilt and anxiety that can kind of revolve around pain what can we do
to help clients guided imagery is generally very helpful if we can help them imagine you know if
that pain in their shoulder imagine the pain is like the color red flowing out of their arm
or other focus mindfulness so you know when you think about something you know when you get a shot
if I don’t think about it it doesn’t hurt near as much as if the nurse says okay now one two three
and you know she’s counting down and I’m getting prepared and I’m focused on it I had
another nurse one time who she was just talking to me and you know put the alcohol on my arm
and just kept on talking and didn’t tell me she was getting ready to give me a shot and before I knew
it she had given me a shot and she was like okay we’re done I’m like you didn’t give me a shot yet
she said yes I did it’s like oh so not focusing on it and next time you have an itch for example
if you’ve ever been driving on the interstate and you can reach on your foot I get those on
the bottom of my foot sometimes and I’m like okay I’m not going to pull over to each my foot if you
focus on something besides the itch eventually, it goes away I’m not saying the pain is gonna completely
go away but the more people focus on it the more it hurts physical therapy can help so encourage
them to get a referral and encourage them to do a self-evaluation if nothing else of ergonomics in
their car at work where they watch TV and spend most of their time at home and they’re sleeping
so those are the four places that they spend most of their time what do their ergonomics look like
and that can help a lot of people mitigate a lot of pain hormones are another thing that
we need to look at imbalances of estrogen and testosterone can contribute to anxiety symptoms
heart palpitations fatigue irritability having people get a physical we can’t as clinicians do
anything about it but doctors can rapid heart weight rate sweating palpitations are not uncommon
in women in perimenopause or menopause so a lot of women start feeling like they’re developing
generalized anxiety and/or something’s going wrong when they start reaching that mid-40s to mid-50s
area and they start having some of these symptoms again we’re not going to diagnose it but we do
want them to recognize that it may not be anything you know is catastrophic this is something that a
a lot of women experience and help them figure out how to deal with that supportive care biologically
now you know this isn’t gonna treat anything but we can help them minimize their vulnerabilities
help them create a sleep routine so their brain and body can rebalance this can help repair any
adrenal issues that may be going on and improve energy levels people with anxiety don’t sleep well
so helping them figure out how to get some quality sleep is important nutrition minimizing caffeine
and other stimulants are going to be a big help because those make people feel anxious and encourage
them to work with a nutritionist to try to prevent spikes and drops in blood sugar which can trigger
the stress response when your blood sugar goes way up or way down you can start getting kind of shaky
and feel weird and that can cause people anxiety because they might think oh my gosh I’m having a
stroke or a heart attack or you know I don’t know what these tremors are so it’s important that
they don’t miss identify symptoms and encourage them to drink enough water dehydration can lead
to toxic Ardea which is increased heart rate sunlight vitamin D deficiency is implicated
in both depression and anxiety mood issues vitamin D has been found in those main areas where
serotonin receptors are found vitamin D receptors are found so we know the serotonin and vitamin D
have something going on sunlight prompts the skin to tell the brain to produce neurotransmitters and
set circadian rhythms which impact the release of serotonin your calming neurochemical melatonin
which is made from breaking down serotonin and helps you sleep and gaba so sunlight actually
helps increase the release of GABA when it’s time to start calming down and going to sleep
exercise studies have shown that exercise can have a relaxing effect and encourage clients to start
slowly there’s not a whole lot of new research on exercise and anxiety aromatherapy has been
used a lot, especially in other countries in the treatment of people with anxiety people with
hospital anxiety people women who are giving birth and they have some birth anxiety there they’ve
been found to be effective in a lot of those studies essential oils for anxiety include
lavender rose Bedevere ylang ylang bergamot chamomile frankincense and Clary sage encourage
clients to just go to a health food store and you know sniff some of these and see if it makes them
feel happy and calm and content the aromatherapy molecules enter the nasal membranes and they
will start triggering neurochemical reactions and so you don’t need to apply it you don’t need
to ingest it all you need to do is so encourage clients if they’re open to it to think about this
because aromatherapy can be integrated into their bedroom for example with an atomizer or a Mr. It
can be incorporated in a lot of different places again where they’re not applying it or ingesting
it in any way all they’re doing is smelling it they’ve used it in defusing aromatherapy in
hospital emergency rooms and they found that it reduces stress and irritability the people in
emergency rooms and I’ve been to enough emergency rooms over the years to know that
people who are in ers typically are not in the best mood so if it can help those people then
it’s probably going to have some sort of an effect so psychologically helping clients realize
that their body thinks there’s a threat for some reason that’s why it triggered the threat response
system which is what they call anxiety so they need to figure out why is there a threat
you know sometimes it’s like the fire alarm going off in my house it just means that the windows are
open and there’s a strong breeze there is no fire there is no problem there’s just a malfunction
it’s a false alarm a lot of times clients get this threat reaction they get this stress
reaction and it’s not a big deal right now so they can start modifying what their brain responds to
and again those basic fears that a lot of people worry about failure rejection loss of control the
unknown and death and loss distress tolerance is one of those cognitive interventions that have
taken center stage in anxiety research and it isn’t about controlling your anxiety you know
helping people recognize their anxiety acknowledge it and say okay I’m anxious it is what it is
how can I improve the next moment instead of saying I’m anxious I shouldn’t be anxious I hate
being anxious and slang with that anxiety let it go just accept it is what it is have the client
learn to start saying I am feeling anxious okay so distracted don’t react because I explain to them
the whole notion of feelings comes in the crest and goes out in about 20 minutes it’s like a wave so once they
acknowledge their feeling if they can distract themselves for twenty or thirty minutes you know
they figured out there was no real threat if they can distract themselves for twenty or
thirty minutes those emotions can go down and then they can deal with it in their wise mind and encourage
them to use distancing techniques instead of saying I am anxious or I am terrified or whatever
have them say I am having the thought that this is the worst thing in the world I am having the
thought that I cannot handle this because thoughts come and go and that comes from acceptance and
commitment therapy functional analysis makes it possible to specify where and when with what frequency
with what intensity and under what circumstances the anxious response is triggered so it’s
important that we help clients develop the ability to do functional analyses on their own so
when they start feeling anxious they can stop and say okay where am I what’s going on how intense
is it what are the circumstances and they start trying to figure out what causes this for
them so they can identify any common themes from their psychoeducation about cognitive distortions
and techniques to prevent those circumstances or mitigate them can be provided so if the client
knows that they get anxious before they go into a meeting with their boss and it’s usually a high
the intensity of anxiety okay so we can educate them and help them identify what fears that may be related
to techniques to slow their breathing and calm their stress reaction and help them figure out
times in the past when they’ve handled going in and talking to their boss and it wasn’t
the end of the world you know there’s lots of different things we can do there for them there
but the first key and it gives them a lot of a huge sense of empowerment to start becoming
detectives in their own life and going okay now under what situations does this happen positive
writing this was another cool study each day for 30 days the experimental group and this
was high school-aged youth in China but you know the experimental group engaged in 20 minutes of
writing about positive emotions they felt that day so they’re writing about anything positive
that make them happy that made them enthusiastic gave them hope whatever long-term expressive
writing positive emotions so after 30 days it appeared to help reduce test anxiety by helping
them develop insight and use positive emotion words so it got them out of the habit of using
the destruction and doom words and encouraged them to get in the habit of looking at the positive
things and being more optimistic it’s a cool activity that clients can try it’s not gonna
hurt anything if you have them journal each day for 30 days mindfulness also came up in the
research and was shown to be effective in a meta-analysis of six articles about mindfulness
based stress reduction four about mindfulness-based cognitive therapy and three about fear of
negative appraisal and emotion regulation were reviewed all of these showed that mindfulness
was an effective strategy for the treatment of mood and anxiety disorders and is an effective
in therapy protocols with different structures including virtual modalities so you know if you’re
doing it via teleconference mindfulness can still be helpful mindfulness helps people start learning
how to observe what’s going on and become aware of what’s going on more aware of those circumstances
which will help them complete their functional analysis but it also helps them become aware of
vulnerabilities and head off things in the past and if they’re taking better care of themselves
that they’re living more mindfully then they may not experience as many situations that trigger
their anxiety mindfulness also encourages clients to learn acceptance that radical acceptance of
it is what it is I’m not gonna fight it I’m angry right now I am anxious right now however I’m
feeling right now is how I feel and that’s okay it’s hard for clients to get to that but once
they get a hold of that and they truly believe it and they can say all right it’s fine I’m not gonna
feel this way forever I’m gonna do something else until the feeling passes it helps and that’s where
the labeling and letting go comes in mindfulness can also help them identify trigger thoughts
what thought were you having right before you started feeling anxious if people are mindful or
let’s start back when people are not mindful they often notice or don’t notice that they’re getting
anxious until they’re like super anxious when people are mindful they become more aware of
subtle cues address unhelpful thoughts when they say or believe it’s a dire necessity for adults
to be loved by significant others for almost everything they do always running gonna happen
why is it a necessity what we can encourage them to do is concentrate on their self-respect
on winning approval for practical purposes you know for promotions or whatever but it’s not about
me being lovable it’s about me getting a promotion and making more money and focusing on loving
rather than being loved because when we give love we generally get love back with unhelpful thought
number two people feel they aren’t able to stand it if things are not the way they want them to be
or are not in their control so encourage clients to focus on the parts that are in their control
and other things in life which are going well and to which they’re committed number three misery
is invariably externally caused and is forced on us by outside people and events just by reading
that makes me feel disempowered so encouraging clients to focus on the fact that reactions such
as misery or happiness are largely caused by the view that people take of the conditions so if
you see it as a tragedy and devastating then it’s probably going to produce misery if you
see it as an opportunity and a challenge it’s probably going to produce a different emotional
reaction if something is or may be dangerous or fearsome people should be upset and
endlessly upset about obsessing about it a lot of people with anxiety get stuck on this you know
if I feel like it’s fearsome I need to worry about it getting on a plane for example if I fear that
that’s dangerous that I need to think about it and worry about it that’s not going to do any
good so encourage clients to figure out how to face it and render it harmless if possible and
when that’s not possible accept the inevitable so looking at airplanes you know facing it means
researching to figure out how dangerous is it really and realizing that it’s not
that dangerous so that helps render it a little bit harmless in their mind it proves to them
that it’s not as dangerous as it could be and when it’s not possible accepting the inevitable you
know you got a fly so getting on there figuring out how you’re gonna get through it hurricanes
are the same way people especially in places like Texas Louisiana Florida may obsess as soon
as it starts coming to hurricane season or if a hurricane is spotted out in the Atlantic somewhere
they start checking the weather every hour or more wondering what the path is going to be and you
know what there’s you can’t change the path of the hurricane so all you can do is board up your house
evacuate if necessary and deal with the fallout child driving is just another example I’ll give
you know my children are learning how to drive and that’s kind of scary and fearsome you know what’s
gonna happen when they’re out there you know you see crashes all the time well render it harmless
by making sure they’ve got good training on how to drive make sure they’re good drivers and then
accepting that some things are just not within my control it’s easier to avoid than face life
difficulties and responsibilities Well running from fear is usually much harder in the long run
so encourage clients to look back at times when they’ve avoided difficulties and responsibilities
and the eventual outcome you know what happened there people believe they should be thoroughly
competent in achieving in all possible respects or they will be isolated rejected and failures we
need to encourage clients to accept themselves as imperfect with human limitations and flaws and
focus on what makes them loveable human being what qualities like courage and intelligence and
creativity and those things that can’t be taken away what inherent qualities do they have that
make them awesome people because something once strongly affected people’s lives they should
indefinitely fear it if you got lost you know when little kids get lost it’s terrifying when
you’re grown up if you get lost you turn on the GPS and you figure out your way but some people
still, you know freaked out about getting lost if they got lost once so we want to help people look
back at past episodes that may be contributing to the current anxiety and compare the situation’s
you know are you the same person or is this not a big deal now that you’re older wiser stronger
encourage them to learn from past experiences but not be overly attached to or prejudiced by
them yeah you could have maybe got lost in the past and it was a horrible experience well you
were six I can see where that would be terrifying and a horrible experience but it doesn’t have to
continue to impact you that way now when you’re you know 26 getting lost you know could be an
opportunity to try a new restaurant or something people must have complete control over things
well this doesn’t happen so encourage clients to remember that the past and the future are
uncontrollable we can’t change the past it is what it is we can learn from it so it doesn’t repeat
but we can’t change it and the future is largely uncontrollable I mean there are a lot of things I
can do to stay moving toward a rich and meaningful life but life is going to throw me curveballs
sometimes and there’s nothing I can do to plan for or control that we can control our actions in the
present to stay on our preferred path and general develop general skills to deal with adversity
should it arise so we want to help clients develop those general problem-solving skills and
the general support system so when they are thrown a curveball you know it doesn’t knock them upside
the head people have virtually no control over their emotions and cannot help feeling disturbed
by things well encourage them to think about the fact that they have real control over destructive
emotions if they choose to work at improving the next moment and changing inaccurate thoughts then
they’re not going to experience the destructive emotions as intensely or as frequently when you
feel an emotion you feel how you feel but again you don’t have to wrestle with it fight it and
nurture it you can say this is how I feel how do I improve the next moment when it comes to
cognitive distortions encourage them to find alternatives when they start to personalize things
if somebody laughs when you walk out of the room then the and the person starts getting anxious
thinking oh they were making fun of me I wonder what they thought I wonder if I had something
stuck to the back of my dress and they start getting all panicked about it that doesn’t do
any good encouraging them to think you know what our three alternate explanations that hadn’t but
had nothing to do with you for why they laughed magnification of the worst thing you know taking
something and saying if this happens then it’s going to be a catastrophe and minimization going
along with that a lot of times when people magnify and see a catastrophe they minimize not only
their strengths and resources but all the other stuff that they’ve got going for them all
they’re seeing is this catastrophe so encouraging them to focus on the facts of what is actually
happening and what is the high probability event and encourage them to get information
and look at the broader picture you know yes you got into a car crash and your car is totaled and
that is unfortunate you know it sucks but you know that is not going to cause you to lose
your job and then become homeless and penniless and yadda-yadda it might cause your insurance to
go up but okay so you don’t have a car but what are the resources that you have who can Who do
you work with that might be able to give you a ride to work you know let’s look at the resources
you have and work around so problem-solving helps with magnification and also focusing on you know
let’s be grateful for what didn’t happen you know you could have been killed but you weren’t the
car was totaled it’s replaceable all or nothing thinking again have them think about what else
could have been happening like Brittney suggested finding the exceptions instead of saying she
always does this look for exceptions when has she not done that what else has she done instead
of this selective abstraction and filtering is when people look for the good the bad and the
ugly a selective abstraction means you kind of see what you expect to see so if you expect
something to be devastating you see only the devastating aspects of it which kind of goes with
the magnification and minimization you filter out the stuff a lot of times when people are in a bad
mood or are anxious they see the negative because that’s the state of mind they’re in so encouraging
people to complete the picture alright there’s all this bad stuff now what’s the good stuff you
know to encourage them to look at the good the bad and the ugly so they get a wide view of exactly
what’s going on and encourage them to remember that hindsight is twenty-twenty when people have
something embarrassing happens or they get anxious about something that happened they look back
and they go I should have or I could have or Oh I wish I wouldn’t have when you were in that
situation you did what you did and you know maybe you may have had a reason for it or you know
you may have not had other options or it may have just been a bonehead thing to do but okay so you
made one mistake hindsight is 2020 that’s gonna that mistake is gonna stand out just like the
great big letter on the eye chart because you’re thinking back and you’re looking at it and that’s
all you see but encouraging clients to remember that other people are too busy worrying about
themselves to remember what they did jumping to conclusions encourages clients to remember to
get all the data if your significant other male significant other comes home and is smelling like
perfume don’t just jump to the conclusion that he was cheating on you maybe he went to the
mall to get a new tie and walked through the perfume area and got spritzed or bought you some
perfume or who knows maybe the person sitting next to him at work sprayed her perfume on the desk
and some of it filtered on there are all different reasons that that might happen so encourage people
to get all the data mind reading we can’t do it you know you can’t read somebody’s mind you don’t
know what they’re thinking so ask them what you think about this don’t assume anything and
emotional reasoning encourages people to step back from a situation and ask themselves am I feeling
anxious about this because I’m feeling anxious and I’m looking for reasons that it should be scary
or am I feeling anxious about this because it’s really scary for some reason there are facts
support my anxiety a lot of times when we go into new situations we may feel anxious because it’s
a new situation but when we step back we say you know what there’s nothing to be worried
about here you know no big deal I got this and move on so instead of rolling with it and trying
to figure out okay I feel anxious so there must be a reason not necessarily very likely a false
alarm other psychological interventions relaxation skills encourage people to learn how to relax
not only physically but mentally diaphragmatic breathing helps encourage them to breathe
through their stomach and put their hand on their belly and feel their belly expand and contract
slows breathing down which triggers the rest and digestion reaction in the brain which is calming
meditation can be helpful for some people some people find trying to quiet their minds too
frustrating because they’ve got too much monkey mind going on that can be later or maybe
never for some people we don’t want to increase their anxiety with interventions cute progressive
muscular relaxation also has a lot of research support and remembers with cute progressive
muscular relaxation we’re Sakura getting them to attach a cue AK you word like relax or breathe
with the relaxation response so they tense their muscles and then relax their muscles and as
they relax their muscles they say their “querk”-word like relaxed and they work from head to toe or
from toe to head tensing and relaxing different muscle groups so they become more aware of what a
tense muscle feels like versus a reactive relaxed muscle there are great scripts that are online
that people have already recorded that can walk people walk clients through CPM are I highly
encourage it because once they get used to it then they can just think that cue they can think
relax and as they exhale they will start to feel their entire body kind of relaxing because it’s
trained when it hears that just like when you hear the word pop quiz when you were in high school
you had a stress reaction well we want to use it in reverse and train the body so that when
it hears a cue word relaxes helps them develop self-esteem because fear of failure and rejection
a lot of times come from needing other people’s approval to help them develop a rational idea of
their real self develops compassion self-talk instead of saying I’m an idiot or I’m stupid or
I’ll never measure up to anything encourage them to talk to themself like they would talk to their
child or hopefully their best friend and encourage them to spotlight strengths whenever they feel
like they’ve got an imperfection to identify these three strengths that they have so they’re you know
balancing out the imperfections and the strengths of cognitive restructuring reframes challenges in
terms of current strengths, not past weaknesses so if you’re going to give a presentation in front
of 60 people and you hate public speaking instead of thinking about you know this is terrifying
because the last time I went up in front of people I forgot everything I was going to say and drop
my note cards well that’s a past weakness what is your current strength you’re prepared you know
the material you Jabba-dada so encourages people to look at all the strengths and resources they
currently have them develop an attitude of gratitude and optimism because like I said with
that the positive writing exercise when people are in a grateful optimistic frame of mind they
tend to see more of the good stuff they see the bad stuff too but they can also see more of the
good stuff and some of the bad stuff they see opportunistically instead of as a devastation
acceptance and commitment therapy says that some of the reasons that we’re miserable are
fear we get fused with our thoughts we think I am terrified well if I am terrified then I can’t
I mean if I am I can’t get rid of anything I am if I’m having the thought that I’m terrified
well I can get rid of a thought I can forget things easily encourage people to evaluate their
experience and empower them to look at things as challenges and opportunities instead of hardships
encourage them not to avoid their experiences so things that are scary gradual exposure and
finding exceptions like for me bridges you know I love public speaking so that’s not a
thing but when I go to a bridge you know when I Drive to the bridge you know when I’m on the
bridge somebody else is driving I get used to doing that when I Drive over a bridge than when
I Drive over one of those bridges that opens up I hate those bridges um I know y’all are just like
oh my gosh yeah it’s an irrational fear I realize that but instead of going straight for the bridge
that opens up going for the little bridges first and then thinking back over times that I’ve gone
over bridges and there’s been no problem you know there are exceptions nothing happened it wasn’t a
big deal Sometimes I didn’t even notice it until somebody pointed out hey look down there at that
pretty water and I’m like oh we’re on a bridge so encourage people to not avoid their experiences
get used to them embrace them and learn that they have the power to deal with them and stop reason
giving for behavior you know use the challenging questions if something is fearsome let’s look for
at the evidence for and against it instead of you know making excuses for social interventions
improve their relationship with their self which goes with self-esteem improvement people are going
to feel less anxious about getting their needs and wants to be met if they know what their needs and wants
are so part of that is becoming mindful cuz a lot of our clients don’t know what they need and want
they just want to feel better but they don’t know how they don’t know what they need to feel
better so helping them identify their needs and wants to encourage them to be their own best friend
you know when they get a promotion take themselves out to dinner pat themselves on the back whatever
it is don’t rely on
other people to do it because other people it’s not that they don’t care but
other people are often very involved in thinking about their stuff and they may not notice
encourage them to develop a method of internal validation so they can feel like they are all
that ‘no bag of chips and they realize why they are lovable human beings and they accept the
the fact that everybody is not going to like them and nobody is gonna like them all the time and
that’s okay you know my kids don’t like me all the time my husband doesn’t like me all the time
I’m okay with that I know I can be challenging but you know most of the time you know they like me
and that’s okay and there are some people you know who don’t like me at all and okay there’s
nothing I can do about that helping our clients develop an okayness with that helps relieve a lot
of anxiety because a lot of people feel like they have to be liked by everybody and if somebody
doesn’t like them it’s like what did I do wrong oh my gosh encourage them to develop healthy
supportive relationships with good boundaries develop assertiveness skills so they can ask for
help when they need it anxiety a lot of times you know that’s the body saying there’s a threat well
if there’s a threat maybe you need some help you know dealing with it so people need to be willing
and able to ask for help and not feel like that’s going to lead them to be rejected and allow them a
certify this will allow them to say no to requests again without feeling like that’s going to result
in them being fully rejected describe the ideal healthy supportive relationship and encourage
them to separate the ideals from the reals you know let’s look at if you had the best relationship
what would it look like okay you know Warden June Cleaver we got that now how realistic is that
you know let’s look at you know rephrasing this a little bit so it’s less extreme you know warden
June Cleaver never fought their kids were perfect you know all those extreme words let’s look at
what’s real what happens in real relationships encourages people to identify who would be
a good partner in supportive relationships I’m not meaning necessarily romantic I’m meaning
friends and where they can be found you know where would you find people that you could be friends
with and encourage them to play through what it means when gaming cuz a lot of times again this
goes with my reading you know what it means when your friend doesn’t return your text right
away what does it mean when your friend cancels dinner on Friday night what does it mean when
you see where I’m going with this and a lot of times clients with anxiety and rejection issues
and low self-esteem will go to the worst-case scenario so encourage them to go back to finding
the exceptions what else could have been happening what else could it be that caused this and it’s
not about you so anxiety is a natural emotion that serves a survival function excessive anxiety can
develop from lack of sleep nutritional problems neurochemical imbalances failure to develop
adequate coping skills cognitive distortions low self-esteem and a variety of other stuff recovery
Ambala involves improving health behaviors making sure your body’s functioning and making the
neurotransmitters it needs and you know release them as needed to identify and build on current
coping strategies address cognitive distortions and develop a healthy supportive relationship with
self and others if you enjoy this podcast please like and subscribe either in your podcast player
or on youtube, you can attend and participate in our live webinars with Dr.

Snipes by subscribing
at all CEUs comm slash counselor toolbox, this episode has been brought to you in part by all
CEUs calmly provide 24/7 multimedia continuing education and pre-certification training to
counselors therapists and nurses since 2006 have used coupon code consular toolbox to get
a 20% discount on your order this month.
As found on YouTubeBrain Booster | Blue Heron Health News ⇝ I was losing my memory, focus – and mind! And then… I got it all back again. Case study:

Brian Thompson There’s nothing more terrifying than watching your brain health fail. You can feel it… but you can’t stop it. Over and over I asked myself, where is this going to end? What am I going to end up like? And nobody could tell me. Doesn’t matter now. I’m over it. Completely well. This is how I did it!
 Which means the brain’s
ability to adjust and adapt as well as learning and memory so these are good receptors I like
them glutamate binds with these receptors and high levels of glutamate are secreted during high
levels of stress glutamate remember is what GABA is made from but high levels of glutamate
it’s an excitatory neural net in the brain and overexposure of neurons to this glutamate can be
excited toxic and may contribute to the loss of neurons in the hippocampus of patients with PTSD
so we’re actually seeing brain volume decrease as a result of exposure to certain chemicals elevated
gluten core glucocorticoid and yeah glucocorticoids increases the sensitivity of these receptors so
you’ve got a bunch of glutamate being dumped and you’ve got a bunch of glucocorticoid you’ve got
cortisol in there making these receptors more sensitive so it’s got they’re more sensitive and
they’ve got more coming in which makes it a whole lot easier to become toxic and start causing
neuronal degradation what does that mean why do we care it may take clients with PTSD more time to
master new skills because of emotional reactivity but also because some of their synaptic plasticity
may be damaged so it may take them a little bit longer to actually acquire and integrate these
new skills it’s not saying they’re stupid they can remember it just fine however when they’re
an emotionally charged state and helping their brain learn that okay this isn’t a threat that’s one
of those sort of subconscious things that has to happen that can take longer if the brain becomes
excited toxic during stress inhibited learning and memory then it becomes excited toxic during
stress which inhibits learning and memory so it’s under stress things are excited toxic neurons
are starting to disappear so I’m wondering and I’m just hypothesizing here I don’t know the
answers obviously or I wouldn’t be practicing it but what happens during the exposure therapies
because that’s exactly what we’re doing is we are flooding the brain with all of these chemicals
and creating basically an excitotoxin now they found some evidence that exposure therapies can
be helpful according to the DOJ website but or not the DOJ I can’t even think of it right
now the VA website but you know I’m wondering long-term what the impact is endogenous opioids
natural painkillers act upon the same receptors activated by exogenous opioids like morphine and
heroin exerts an inhibitory influence on the HPA axis well we know that people take opiates
and it has depressant effects on them it slows them down and calms them down alterations in our
natural opioids may be involved in certain PTSD symptoms such as numbing stress-induced analgesia
and dissociation again think of any clients you’ve had who have been abused or even taken and not like
the side effects of opiates are what opiates do to some people make them feel more relaxed stress
induced and analgesia they don’t have as much physical pain sometimes they just it’s there
I don’t care pill another interesting factor is now truck zone which is used to oppose opiate
appears to be effective in treating symptoms of dissociation flashbacks in traumatized persons so
basically, they’re saying if we undo the endogenous opioids we can treat these symptoms it highlights
the risk of opiate abuse for persons with PTSD though because if endogenous opioids produce
some of these numbing symptoms and dissociative symptoms so they can get away from the pain and
the flashbacks then if they add to that you know oral opioids it could prove to be a very tempting
cocktail we do want to as clinicians figure out how we can assist them with their physical and
emotional distress tolerance so they don’t feel the need to numb and escape and you know I
can’t imagine what some people have seen have gone through and I’m not trying to take that away
from them, I’m trying to help them figure out how they can stay present and learn to integrate it
changes question marks in brain structure and one of the questions that’s come up in the research is
because there aren’t any longitudinal studies that looked at it was the hippocampal volume as low to
begin with which created a predisposition for PTSD or did PTSD create the smaller hippocampal volume
interesting hippocampus is implicated in the control of stress responses memory and contextual
aspects of fear conditioning so it helps you to find these triggers in the environment that
help you become aware with your senses about when there might be a trauma prolonged exposure
to stress and high levels of glucocorticoids damage the hippocampus we’ve talked about that
hippocampal volume reduction in PTSD may reflect the accumulated toxic effects of repeated exposure
to increased cortisol levels what I called earlier the flatter the Furious having you know your body
holding on to cortisol for this extreme stress and then when it perceives stress it’s either
nothing or it’s extreme there are no kind sort of mild stressors out there that decrease hippocampal
volumes might also be a pre-existing vulnerability factor for developing PTSD the amygdala yet
another brain structure is the Olympic structure involved in the emotional process and it’s
critical for the acquisition of fear responses functional imaging of studies has revealed hyper
responsiveness and PTSD during the presentation of stressful script cues or trauma reminders but
also patients show increased amygdala responses to general emotional stimuli that are not trauma
associated such as emotional faces so they show an increased responsivity to things they see on the
TV that aren’t trauma-related to people crying to people showing anger’s going to have a
stronger emotional amygdala response than people without PTSD so clients with PTSD may be more
emotionally responsive across the board leading to more emotional dysregulation again an area that
we can help provide them with tools for early adverse experiences including prenatal stress and stress
throughout childhood has profound and long-lasting effects on the development of neurobiological
symptoms the brain is developing and if is exposed to a lot of stress and some of these excited toxic
situations how does that differ in the amount of damage caused versus a brain that’s already kind
of pretty much-formed programming may change for subsequent stress reactivity and vulnerability
to develop PTSD so if these happen during childhood or at any time the brain can
basically reprogram and go that it’s a really dangerous place out there so I need to hold
on to cortisol and I need to hold on to these stress hormones because every time I turn around
it seems like there’s a threat so I am going to be hyper-vigilant and respond in an exaggerated way
to protect you from the outside world adult women with childhood trauma histories have been shown
to exhibit sensitization of both neuroendocrine and Audino stress responses so basically they’re
showing hypo cortisol ISM a variety of changes take place in the brains and nervous systems of
people with PTSD and we talked about a lot of those the key take-home point is stress can
actually get toxic in the brain and cause physical changes not just thought changes in the brain
preexisting issues causing hypo cortisol ism where the brain has already downregulated whether it’s
due to chronic illness or chronic psychological stress increases the likelihood of the development
of PTSD this points to the importance of prevention and early intervention of adverse
childhood experiences we really need to get in there and help these people develop distress
tolerance skills understanding of vulnerabilities so they’re not going from flat to furious all
the time and so that they can understand why their body kind of responds and why they respond
differently than others and you know as we talk about this and of course I’m regularly bringing up
DBT buzzwords if you will think about your clients if you’ve worked with any who’ve had borderline
personality disorder what kind of history do they have did they have just a great childhood no we
know that people with BPD generally had pretty chaotic childhoods so this research is also
kind of underscoring why they may react and act the way they do that flat to furious people with
hypo cortical ism may or may not have PTSD so we don’t want to say well you’re fine if you don’t
have PTSD symptoms we do know that every trauma potentially can cause the body to down-regulate
and I kind of look at it as conserving a little bit more of the energy that it needs each time so
instead of conserving 60% now it’s conserving 65 and 66 each time it encounters a stressor in order
to prepare for potential ongoing threats in the environment hypercortisolism sets the stage for
the flattened the furious leading to toxic levels of glutamate upon exposure to stressors which
can cause the theorized reduction in hippocampal volume and persistent negative brain changes now I
always say the brain can you know rebalance itself and all well that’s part of the plasticity that is
the really cool thing about our brain however as far as regenerating those neurons I haven’t found
any evidence in the research that we found a way to help people regenerate once we’ve already those
neurons are gone they’ve been killed off the brain has to find a workaround so it does take time
but I do believe people can minimize some of the impact of the trauma they may have experienced
people with PTSD are more reactive to emotional stimuli even stimuli unrelated to trauma again
think about some of your clients especially if you work in a residential situation where you’re
around on 24/7, you know for 30 or 60 days, and you may see some clients that seem to get upset
over everything and you’re like ah such a drama queen or such a drama king and to yourself not
to anybody else but when you think about it from this perspective it gives you a different
perspective and you might say oh maybe their body responds differently they’ve got more emotional
dysregulation because of prior trauma they’re not trying to overreact this is their body’s response
because it’s perceived threat so many times it gives me a different approach to working
with that client hypercortisolism results when the brain perceives that continued effort is futile
feelings of fatigue set in akin to reduced stress tolerance so think about you know when you’ve had
a really long stressful period you know weeks or months maybe you’re dealing with an ailing family
member or something it’s just a lot of stress and you start getting really tired and when you’re
really tired and you’re worn down and somebody gives you one more thing it’s that one more thing
normally wouldn’t bother you but right now you just can’t take it so we can see how there’s a
reduced stress tolerance when somebody’s already at this stage reducing fatigue in our clients can
be accomplished in part with psychological factors including motivation or knowledge of other people
who are dealing with similar things support groups feedback about their and making sure they have
frequent successes not once a week but I want to have them keep a journal every day of something
good that happened or something positive that may indicate they’re moving forward in their
treatment goals and knowledge of an endpoint.
Which means the brain’s
ability to adjust and adapt as well as learning and memory so these are good receptors I like
them glutamate binds with these receptors and high levels of glutamate are secreted during high
levels of stress glutamate remember is what GABA is made from but high levels of glutamate
it’s an excitatory neural net in the brain and overexposure of neurons to this glutamate can be
excited toxic and may contribute to the loss of neurons in the hippocampus of patients with PTSD
so we’re actually seeing brain volume decrease as a result of exposure to certain chemicals elevated
gluten core glucocorticoid and yeah glucocorticoids increases the sensitivity of these receptors so
you’ve got a bunch of glutamate being dumped and you’ve got a bunch of glucocorticoid you’ve got
cortisol in there making these receptors more sensitive so it’s got they’re more sensitive and
they’ve got more coming in which makes it a whole lot easier to become toxic and start causing
neuronal degradation what does that mean why do we care it may take clients with PTSD more time to
master new skills because of emotional reactivity but also because some of their synaptic plasticity
may be damaged so it may take them a little bit longer to actually acquire and integrate these
new skills it’s not saying they’re stupid they can remember it just fine however when they’re
an emotionally charged state and helping their brain learn that okay this isn’t a threat that’s one
of those sort of subconscious things that has to happen that can take longer if the brain becomes
excited toxic during stress inhibited learning and memory then it becomes excited toxic during
stress which inhibits learning and memory so it’s under stress things are excited toxic neurons
are starting to disappear so I’m wondering and I’m just hypothesizing here I don’t know the
answers obviously or I wouldn’t be practicing it but what happens during the exposure therapies
because that’s exactly what we’re doing is we are flooding the brain with all of these chemicals
and creating basically an excitotoxin now they found some evidence that exposure therapies can
be helpful according to the DOJ website but or not the DOJ I can’t even think of it right
now the VA website but you know I’m wondering long-term what the impact is endogenous opioids
natural painkillers act upon the same receptors activated by exogenous opioids like morphine and
heroin exerts an inhibitory influence on the HPA axis well we know that people take opiates
and it has depressant effects on them it slows them down and calms them down alterations in our
natural opioids may be involved in certain PTSD symptoms such as numbing stress-induced analgesia
and dissociation again think of any clients you’ve had who have been abused or even taken and not like
the side effects of opiates are what opiates do to some people make them feel more relaxed stress
induced and analgesia they don’t have as much physical pain sometimes they just it’s there
I don’t care pill another interesting factor is now truck zone which is used to oppose opiate
appears to be effective in treating symptoms of dissociation flashbacks in traumatized persons so
basically, they’re saying if we undo the endogenous opioids we can treat these symptoms it highlights
the risk of opiate abuse for persons with PTSD though because if endogenous opioids produce
some of these numbing symptoms and dissociative symptoms so they can get away from the pain and
the flashbacks then if they add to that you know oral opioids it could prove to be a very tempting
cocktail we do want to as clinicians figure out how we can assist them with their physical and
emotional distress tolerance so they don’t feel the need to numb and escape and you know I
can’t imagine what some people have seen have gone through and I’m not trying to take that away
from them, I’m trying to help them figure out how they can stay present and learn to integrate it
changes question marks in brain structure and one of the questions that’s come up in the research is
because there aren’t any longitudinal studies that looked at it was the hippocampal volume as low to
begin with which created a predisposition for PTSD or did PTSD create the smaller hippocampal volume
interesting hippocampus is implicated in the control of stress responses memory and contextual
aspects of fear conditioning so it helps you to find these triggers in the environment that
help you become aware with your senses about when there might be a trauma prolonged exposure
to stress and high levels of glucocorticoids damage the hippocampus we’ve talked about that
hippocampal volume reduction in PTSD may reflect the accumulated toxic effects of repeated exposure
to increased cortisol levels what I called earlier the flatter the Furious having you know your body
holding on to cortisol for this extreme stress and then when it perceives stress it’s either
nothing or it’s extreme there are no kind sort of mild stressors out there that decrease hippocampal
volumes might also be a pre-existing vulnerability factor for developing PTSD the amygdala yet
another brain structure is the Olympic structure involved in the emotional process and it’s
critical for the acquisition of fear responses functional imaging of studies has revealed hyper
responsiveness and PTSD during the presentation of stressful script cues or trauma reminders but
also patients show increased amygdala responses to general emotional stimuli that are not trauma
associated such as emotional faces so they show an increased responsivity to things they see on the
TV that aren’t trauma-related to people crying to people showing anger’s going to have a
stronger emotional amygdala response than people without PTSD so clients with PTSD may be more
emotionally responsive across the board leading to more emotional dysregulation again an area that
we can help provide them with tools for early adverse experiences including prenatal stress and stress
throughout childhood has profound and long-lasting effects on the development of neurobiological
symptoms the brain is developing and if is exposed to a lot of stress and some of these excited toxic
situations how does that differ in the amount of damage caused versus a brain that’s already kind
of pretty much-formed programming may change for subsequent stress reactivity and vulnerability
to develop PTSD so if these happen during childhood or at any time the brain can
basically reprogram and go that it’s a really dangerous place out there so I need to hold
on to cortisol and I need to hold on to these stress hormones because every time I turn around
it seems like there’s a threat so I am going to be hyper-vigilant and respond in an exaggerated way
to protect you from the outside world adult women with childhood trauma histories have been shown
to exhibit sensitization of both neuroendocrine and Audino stress responses so basically they’re
showing hypo cortisol ISM a variety of changes take place in the brains and nervous systems of
people with PTSD and we talked about a lot of those the key take-home point is stress can
actually get toxic in the brain and cause physical changes not just thought changes in the brain
preexisting issues causing hypo cortisol ism where the brain has already downregulated whether it’s
due to chronic illness or chronic psychological stress increases the likelihood of the development
of PTSD this points to the importance of prevention and early intervention of adverse
childhood experiences we really need to get in there and help these people develop distress
tolerance skills understanding of vulnerabilities so they’re not going from flat to furious all
the time and so that they can understand why their body kind of responds and why they respond
differently than others and you know as we talk about this and of course I’m regularly bringing up
DBT buzzwords if you will think about your clients if you’ve worked with any who’ve had borderline
personality disorder what kind of history do they have did they have just a great childhood no we
know that people with BPD generally had pretty chaotic childhoods so this research is also
kind of underscoring why they may react and act the way they do that flat to furious people with
hypo cortical ism may or may not have PTSD so we don’t want to say well you’re fine if you don’t
have PTSD symptoms we do know that every trauma potentially can cause the body to down-regulate
and I kind of look at it as conserving a little bit more of the energy that it needs each time so
instead of conserving 60% now it’s conserving 65 and 66 each time it encounters a stressor in order
to prepare for potential ongoing threats in the environment hypercortisolism sets the stage for
the flattened the furious leading to toxic levels of glutamate upon exposure to stressors which
can cause the theorized reduction in hippocampal volume and persistent negative brain changes now I
always say the brain can you know rebalance itself and all well that’s part of the plasticity that is
the really cool thing about our brain however as far as regenerating those neurons I haven’t found
any evidence in the research that we found a way to help people regenerate once we’ve already those
neurons are gone they’ve been killed off the brain has to find a workaround so it does take time
but I do believe people can minimize some of the impact of the trauma they may have experienced
people with PTSD are more reactive to emotional stimuli even stimuli unrelated to trauma again
think about some of your clients especially if you work in a residential situation where you’re
around on 24/7, you know for 30 or 60 days, and you may see some clients that seem to get upset
over everything and you’re like ah such a drama queen or such a drama king and to yourself not
to anybody else but when you think about it from this perspective it gives you a different
perspective and you might say oh maybe their body responds differently they’ve got more emotional
dysregulation because of prior trauma they’re not trying to overreact this is their body’s response
because it’s perceived threat so many times it gives me a different approach to working
with that client hypercortisolism results when the brain perceives that continued effort is futile
feelings of fatigue set in akin to reduced stress tolerance so think about you know when you’ve had
a really long stressful period you know weeks or months maybe you’re dealing with an ailing family
member or something it’s just a lot of stress and you start getting really tired and when you’re
really tired and you’re worn down and somebody gives you one more thing it’s that one more thing
normally wouldn’t bother you but right now you just can’t take it so we can see how there’s a
reduced stress tolerance when somebody’s already at this stage reducing fatigue in our clients can
be accomplished in part with psychological factors including motivation or knowledge of other people
who are dealing with similar things support groups feedback about their and making sure they have
frequent successes not once a week but I want to have them keep a journal every day of something
good that happened or something positive that may indicate they’re moving forward in their
treatment goals and knowledge of an endpoint. Where are we going with this when is the treatment
going to end I don’t want most clients don’t want to be with us forever no matter how lovable
we are do you want to feel better and be done with us so having to help them see that there
is an endpoint we’re going to accomplish this goal this month and then we can reassess 46% of
people in the US are exposed to adverse childhood experiences so like I said this is a huge area
for early intervention where we can prevent people from developing PTSD later in life how awesome
would that be instruction and skills to handle emotional dysregulation including mindfulness
vulnerability prevention and awareness emotion regulation distress tolerance and problem-solving
could be wonderful additions to health curriculums anything any skills groups you do with children
or adolescents or even adults I mean just because they’re adults doesn’t mean that they’re safe
from PTSD or that they’ve crossed any threshold where they’re too old to learn we’re never too
old to learn of those exposed to trauma education about and normalization of their heightened
emotional reactivity and susceptibility to PTSD in the future may be helpful in increasing their
motivation for their current treatment protocol whatever it is but it also just normalizes things
so they don’t feel like they’re overreacting or they don’t feel guilty for being so tired
or whatever they’re experiencing right now are there any questions I know I went through
a lot of really complicated stuff but I thought it was really interesting not only the way
our brain reacts in order to protect us but how cross-cutting a lot of this stuff
was it not just PTSD we’re talking about necessarily but a lot of this information
applies to our clients with chronic fatigue burnout and chronic stress and we can
see that those people also are at risk at higher risk of PTSD should they be exposed
to trauma and none of us is immune I mean there are tornadoes there are hurricanes
there are you know things that happen that really stink so the more we can help clients
be aware of things develop skills and tools to prevent as much harm as possible I
think the more effective we are as clinicians depending on the client and I can do some
more research on the VA website because they’re really into medications for PTSD I
know ketamine which is a horse tranquilizer has been shown to be effective in people
with PTSD and there have been some others that have kind of given me pause ketamine
is a hypnotic you know most of the drugs they’re trying out right now are really in my
opinion they’re powerful drugs but a lot of them all of them that I know of have
pretty high addictive potentials too so they make me nervous but you know when you’re
weighing the when you’re going from a harm reduction model that’s not necessarily not
necessarily such the be-all-end-all I guess that’s interesting that you use ketamine in the ER it’s definitely powerful effective stuff and like I said earlier some of the
stuff that some of my clients and some people have seen done experienced I couldn’t even
imagine and you know sometimes for them to actually survive we may need to look at some
of these more intense more powerful drugs PTSD and veteran trauma is not are not my focus
right now and yes marijuana is being experimented with or looked at used whatever however you want
to look at it for PTSD treatment with veterans there’s pretty much not a drug out there they
haven’t tried to throw at it to see well what will this do I believe they were even using
LSD experimentally for a little while too you the VA I mean if you’re interested in this
topic let me see if I could pull that down into here, we go to the National Center
for PTSD US Department of Veterans Affairs has a lot of information if you go for
professionals, it has a ton more information if you can get on get some of your SI CEUs on
demand they do have some free CEUs for PTSD here I’ve never taken any of them but what
I’ve looked at when I’ve looked at like the PowerPoints the presentations and stuff I’m
sure they’re good so if you’re you do focus a lot on PTSD and you can get on-demand CEUs
then this might be a place to get some good free ones aside from DBT are there any other
evidence-based practices for therapy that you’ve seen work best in combination with the
medications cognitive processing therapy when you’re working specifically with veterans
and there is a free course on that too and this one I have gone through
and it’s really awesome CPT dot must seed and here I’ll just put it
into that education and this is a free course oops and here’s the other one ah golly everyone and
embryo does have a lot of research effectiveness with people with PTSD too so yes I would
definitely encourage people to explore all options alrighty everybody I really
appreciate you coming today and sticking with me through this topic and I will see
you on Thursday if you have any questions please feel free to email me or you can
always also send it to support that all CEUs com either way I get it and otherwise I
will see you on Tuesday thanks a bunch if you enjoy this podcast please like and
subscribe either in your podcast player or on YouTube you can attend and participate
in our live webinars with Doctor Snipes by subscribing at all CEUs comm slash
counselor toolbox this episode has been brought to you in part by all CEUs
com providing 24/7 multimedia continuing education and pre-certification training to
counselors therapists and nurses since 2006 used coupon code consular toolbox to get
a 20% discount on your order this monthAs found on YouTube15 Modules Of Intimate Video Training With Dr. Joe Vitale – You’re getting simple and proven steps to unlock the Awakened Millionaire Mindset: giving you a path to MORE money, …
Where are we going with this when is the treatment
going to end I don’t want most clients don’t want to be with us forever no matter how lovable
we are do you want to feel better and be done with us so having to help them see that there
is an endpoint we’re going to accomplish this goal this month and then we can reassess 46% of
people in the US are exposed to adverse childhood experiences so like I said this is a huge area
for early intervention where we can prevent people from developing PTSD later in life how awesome
would that be instruction and skills to handle emotional dysregulation including mindfulness
vulnerability prevention and awareness emotion regulation distress tolerance and problem-solving
could be wonderful additions to health curriculums anything any skills groups you do with children
or adolescents or even adults I mean just because they’re adults doesn’t mean that they’re safe
from PTSD or that they’ve crossed any threshold where they’re too old to learn we’re never too
old to learn of those exposed to trauma education about and normalization of their heightened
emotional reactivity and susceptibility to PTSD in the future may be helpful in increasing their
motivation for their current treatment protocol whatever it is but it also just normalizes things
so they don’t feel like they’re overreacting or they don’t feel guilty for being so tired
or whatever they’re experiencing right now are there any questions I know I went through
a lot of really complicated stuff but I thought it was really interesting not only the way
our brain reacts in order to protect us but how cross-cutting a lot of this stuff
was it not just PTSD we’re talking about necessarily but a lot of this information
applies to our clients with chronic fatigue burnout and chronic stress and we can
see that those people also are at risk at higher risk of PTSD should they be exposed
to trauma and none of us is immune I mean there are tornadoes there are hurricanes
there are you know things that happen that really stink so the more we can help clients
be aware of things develop skills and tools to prevent as much harm as possible I
think the more effective we are as clinicians depending on the client and I can do some
more research on the VA website because they’re really into medications for PTSD I
know ketamine which is a horse tranquilizer has been shown to be effective in people
with PTSD and there have been some others that have kind of given me pause ketamine
is a hypnotic you know most of the drugs they’re trying out right now are really in my
opinion they’re powerful drugs but a lot of them all of them that I know of have
pretty high addictive potentials too so they make me nervous but you know when you’re
weighing the when you’re going from a harm reduction model that’s not necessarily not
necessarily such the be-all-end-all I guess that’s interesting that you use ketamine in the ER it’s definitely powerful effective stuff and like I said earlier some of the
stuff that some of my clients and some people have seen done experienced I couldn’t even
imagine and you know sometimes for them to actually survive we may need to look at some
of these more intense more powerful drugs PTSD and veteran trauma is not are not my focus
right now and yes marijuana is being experimented with or looked at used whatever however you want
to look at it for PTSD treatment with veterans there’s pretty much not a drug out there they
haven’t tried to throw at it to see well what will this do I believe they were even using
LSD experimentally for a little while too you the VA I mean if you’re interested in this
topic let me see if I could pull that down into here, we go to the National Center
for PTSD US Department of Veterans Affairs has a lot of information if you go for
professionals, it has a ton more information if you can get on get some of your SI CEUs on
demand they do have some free CEUs for PTSD here I’ve never taken any of them but what
I’ve looked at when I’ve looked at like the PowerPoints the presentations and stuff I’m
sure they’re good so if you’re you do focus a lot on PTSD and you can get on-demand CEUs
then this might be a place to get some good free ones aside from DBT are there any other
evidence-based practices for therapy that you’ve seen work best in combination with the
medications cognitive processing therapy when you’re working specifically with veterans
and there is a free course on that too and this one I have gone through
and it’s really awesome CPT dot must seed and here I’ll just put it
into that education and this is a free course oops and here’s the other one ah golly everyone and
embryo does have a lot of research effectiveness with people with PTSD too so yes I would
definitely encourage people to explore all options alrighty everybody I really
appreciate you coming today and sticking with me through this topic and I will see
you on Thursday if you have any questions please feel free to email me or you can
always also send it to support that all CEUs com either way I get it and otherwise I
will see you on Tuesday thanks a bunch if you enjoy this podcast please like and
subscribe either in your podcast player or on YouTube you can attend and participate
in our live webinars with Doctor Snipes by subscribing at all CEUs comm slash
counselor toolbox this episode has been brought to you in part by all CEUs
com providing 24/7 multimedia continuing education and pre-certification training to
counselors therapists and nurses since 2006 used coupon code consular toolbox to get
a 20% discount on your order this monthAs found on YouTube15 Modules Of Intimate Video Training With Dr. Joe Vitale – You’re getting simple and proven steps to unlock the Awakened Millionaire Mindset: giving you a path to MORE money, …
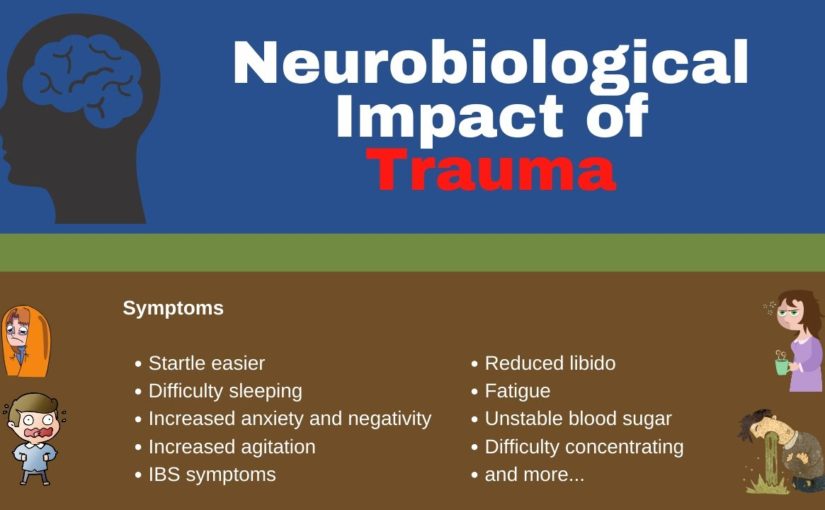
 The Market WeekSign Up For The Free Newsletter No nonsense, no spam, unsubscribe anytime You can unsubscribe at any time. Read our privacy policy. Financial disclaimer: The Market Week is a general interest newsletter that is not liable for the suitability or future investment performance of any securities or strategies discussed. Readers are advised that the material contained herein should be used solely for informational purposes. As a financial newsletter publisher of general and regular circulation, we cannot tender individual investment advice. Read our full disclaimer.
The Market WeekSign Up For The Free Newsletter No nonsense, no spam, unsubscribe anytime You can unsubscribe at any time. Read our privacy policy. Financial disclaimer: The Market Week is a general interest newsletter that is not liable for the suitability or future investment performance of any securities or strategies discussed. Readers are advised that the material contained herein should be used solely for informational purposes. As a financial newsletter publisher of general and regular circulation, we cannot tender individual investment advice. Read our full disclaimer. 
 Snipes by subscribing
at all CEUs comm slash counselor toolbox, this episode has been brought to you in part by all
CEUs calmly provide 24/7 multimedia continuing education and pre-certification training to
counselors therapists and nurses since 2006 have used coupon code consular toolbox to get
a 20% discount on your order this month.
Snipes by subscribing
at all CEUs comm slash counselor toolbox, this episode has been brought to you in part by all
CEUs calmly provide 24/7 multimedia continuing education and pre-certification training to
counselors therapists and nurses since 2006 have used coupon code consular toolbox to get
a 20% discount on your order this month.





















 Snipes by subscribing
at all CEUs comm slash counselor toolbox, this episode has been brought to you in part by all
CEUs calmly provide 24/7 multimedia continuing education and pre-certification training to
counselors therapists and nurses since 2006 have used coupon code consular toolbox to get
a 20% discount on your order this month.
Snipes by subscribing
at all CEUs comm slash counselor toolbox, this episode has been brought to you in part by all
CEUs calmly provide 24/7 multimedia continuing education and pre-certification training to
counselors therapists and nurses since 2006 have used coupon code consular toolbox to get
a 20% discount on your order this month.
 Etc sometimes you need to
delay joint sessions until the parent or caregiver can offer the child support and sometimes that
means not even starting treatment really until the parent and caregiver parent or caregiver
can be on board now you can get started with psychoeducation emotions identification feelings
identification and stress management and coping skills you know there were not really
poking a bunch of bears so you can probably safely get started on that if it’s sometimes it’s
court-ordered and they have to start treatment by April 1st or something so there are things you can
do but you may need to delay the actual beginning of the trauma narrative until the parent is
able to be available to educate everybody on how therapy works and instill in everyone not just
the parent optima optimist that well optimism about the child’s potential for recovery you
know sometimes they’ve been dealing with this child’s acting out behaviors for so long they’re
just like you know we’ve already been to three other therapists I don’t know what’s going to
fix it or I’ve done everything I know how to do good luck so we can talk about you know a
different approach or we can talk about what they’ve done that’s worked for a short period
of time and build on those strengths to instill optimism and hope and empowerment so
initially, when we talk about psycho-education it’s important to provide accurate information
about the trauma when children are traumatized they can be confused and not completely understand
what happened they may blame themselves and they may hold on to myths because they’ve been misled
and/or deliberately given incorrect information so one of the best ways we can help is to correct
that information provides information about how often this happens and whether you know it’s okay
to do this that or the other psychoeducation clarifies inappropriate information children may
have obtained directly from the perpetrator or on their own so the perpetrator may have told them
that this is how I express love or this is how you need to be disciplined because you don’t learn
this is how I was disciplined whatever it is or they could have gotten it on their own they could
have gotten it from school from the internet or just come up with it in their little heads trying
to make sense of what happened psychoeducation also helps them identify safety issues the
difference between safe situations and dangerous situations and as we get through this I really
want you to get away from the notion that TF CBT and childhood trauma are only physical and sexual
abuse there are so many other traumas as evidenced by the adverse childhood experiences survey that
I want you to wrap your head around that and there are things they didn’t cover in the aces such as
bullying and natural disasters so we want to help children whatever the trauma is the trauma made
they feel unsafe so we want to identify safety issues if the trauma was a hurricane then we want
to talk about what hurricanes are how often they hit what to safety plan etc so every time a
the thunderstorm comes they don’t freak out and we want to use psychoeducation to provide another
way to target faulty or maladaptive beliefs by helping to normalize thoughts and feelings about
the traumatic experience you know it makes sense that that was scary and makes sense that
you’re angry it makes sense that you feel this way and we can talk about why that makes
sense and why it makes you feel that way through cycle education you’re getting the child to start
talking about the specific trauma that he or she experienced in a less anxiety-provoking way by
talking in Jen wrong about the type of trauma so you’re talking about natural disasters you’re
talking about plane crashes you’re talking about domestic violence so they start learning about
it and then eventually you’re going to move down to their experience with it so like I said there
are a ton of different traumas and the ACE study even acknowledges that these are just the ten most
common ones that they heard however there are many many many different traumas and types of trauma
some of the biggest ones are physical and sexual abuse physical neglect emotional abuse
and neglect and the Aces identified mother treated violently I would say anyone in the household
treated violently it’s not just the mother’s substance misuse within the household and that
can be by the parents or by siblings household mental illness parental separation or divorce and
an incarcerated household member so those were aces but then like I said there’s also bullying
the death of a parent or sibling is extremely traumatic hurricane tornado natural disaster and
then I put the fire out separately because sometimes fire can be man-made sometimes it can be a wiring
problem but sometimes it can be Jr was playing with matches now even if jr. Accidentally started
the fire does that make it any less traumatic no it probably makes it more traumatic because then
there’s a whole sense of guilt and responsibility but it’s still a trauma that has to be dealt
with so I put a link to the adverse childhood experiences website if you want to go look more
about that but we’re going to move on psycho-education involves specific information about
the traumatic events the child has experienced not the child’s event we’re not going to go
into police records or something, we’re just going to talk about specific information about
domestic violence or whatever body awareness and sex education in cases of physical or sexual
maltreatment and there are caveats for getting parental consent and permission and all that other
stuff and Risk Reduction skills to decrease the risk of future traumatization now going back to
those other things it’s not just about physical or sexual abuse so we want to look at what was the
the risk created by you know how can you reduce your risk of being bullied how can you reduce your
risk of being traumatized in a tornado you know you can’t stop the tornado from coming
and they’re everywhere so what do you do and talk about a safety plan the same thing with fire
information needs to be tailored to fit a child’s particularly particular experiences and level
of knowledge obviously, you’re going to provide different information to a seven-year-old than
you are to a 17-year-old provide caregivers with handout materials to reinforce the information
discussed in session so this may help educate the parents about some of it but it lets them
know what you talked about and it gets us all on the literal same page you’re providing them a
handout of everything you went over with Junior and we want to encourage caregivers to discuss
this information at home reinforces accurate information about how safe or unsafe they
are and obviously, we’re going towards safe and reinforced accurate information and develop
a safety plan so they feel confident that at home they’re going to be taken care of when you
start psychoeducation you do want to get a sense of what the child already knows and you can use
a question-and-answer game format in which the child gets points for answering questions which I
love this suggestion so you can ask them if you know what is a hurricane or is a tornado and see
if they know and see if they know how much time and much-advanced warning we have for a tornado
versus a hurricane or you know whatever situation you’re talking about you see I did a lot of posts
Hurricane Katrina counseling in northern Florida so that’s one of those things that comes up for
I am talking with children about how likely is it that a category 5 hurricane is going to hit
again but encouraging them to give your aunt’s give answers and if they give the wrong answer you
know it’s great to try now you know try to coach them into a correct answer or provide them the correct
one but give them credit for at least making an effort sample questions might include what is
you know and put in the type of trauma what is bullying how often do you think bullying happens
and why does bullying happen you know those are some questions you can ask to just open a dialogue
about bullying, if this child has been a victim of bullying and is and is traumatized so cultural
considerations meet the child and family where they are by presenting information in a way which
they can relate it to their belief system and you may need to consult with their spiritual
guidance guides leaders whether it be a pastor or you know whatever to get some guidance
on how to handle certain aspects of whether it was the will of God and in the case of sexual abuse
how to handle the concept of virginity and how to handle the concept of bad things happening to bad
people and whatever else they think is coming from or their parents are instilling in them in a
belief system we want to make sure that we’re not necessarily contradicting it and going oh mom dad
and the church is wrong but we also want to help them try to integrate this in a way that can help
they have strong self-esteem so reaching out to those spiritual leaders and the family asking what
their belief system about certain things can be very helpful assess the general beliefs about
the trauma if something happened or when something happens ask the parent or the family that’s there
not necessarily the child but you want to get a sense of what the family stance is on why this
happened what it means how it’s going to impact life hence foreign henceforth and forever more
focus on the events they perceive as traumatic to the family but most especially the child if the
child’s going back to the Aces you know maybe the parents got divorced but the child doesn’t
see that as traumatic because there was domestic violence ahead of time the domestic violence was
traumatic the divorce was a relief so wherever the child is with each trauma we want to
be respectful of what they perceive is traumatic and tailor the information so the family can be
more receptive to it as supportive as possible and sometimes you need to make sure that the language
you know make sure the language is not jargony about general views of mental health and mental health
treatment should also be assessed and addressed in the psychoeducation piece not only with the child
but also with the family, if they are suspicious of it don’t understand it think that you’re just
going to magically fix Junior we want to demystify the process and talk about what is the purpose of
the assessment what is the purpose of each one of these activities and why am I doing this or why
are we doing this as a team and how can it help and then we also want to provide information to
D stigmatize and normalize mental health issues and seeking treatment some cultures are still
resistant to seeking treatment and I use the term cultures broadly because there’s
a stigma associated with it so normalizing for them how many people go to treatment how common
PTSD is or whatever the situation you’re dealing with it doesn’t mean they have to like it but at
At least it will give them a little bit of a nugget to understand that they’re not the only ones if
they are from a cultural group a minority cultural group of some sort you might want to provide
information about how common this particular issue is in their group I’ve done a lot of work
with law enforcement and emergency responders and they’re kind of their little group so
we talk about how common depression is among law enforcement and emergent emergency responders
specifically, because they face so much so many different stressors than you know Joe Schmo over
here so it D stigmatizes and normalizes a little bit now they still may not talk about it and
go well hey you know 37% of us have clinical depression no that’s probably not going to happen
but at least in the back of their mind, they can go you know what I’m looking around this room and
I can bet that at least one other person’s on antidepressants or something and feel a little
less unique and isolated in parent sessions you want to provide a rationale and overview of the
treatment model educates parents about the trauma and talks about the child’s trauma-related symptoms
so we’re going to go over what is hyper-vigilance what is the function it why people become
hypervigilant after trauma and what might it look like in a child because it presents very
differently for different children so we might want to give some ideas and say does this sound
like Johnny or does this sound like Johnny and help them understand why these behaviors may
be coming out we want to talk about how early treatment helps prevent long-term problems okay
maybe the trauma happened three years ago but still, it’s better than waiting ten more years and
you know Johnny’s still not having any Ellucian will want to talk about the importance of talking
directly about the trauma to help the children cope with their experiences and not hedging and
this will be on a case-by-case basis but the manual walks you through handling this discussion with
the parents about exactly how much detail do I go into if Johnny brings it up at home reassure
parents that children will first be taught skills to help them cope with their discomfort
and that talking about the trauma will be done slowly with a great deal of support so we’re not
just going to plop them down and go okay and tell me about the day that all this happened which
is what the child has experienced already if it was reported to law enforcement and/or the child
welfare they’ve probably had somebody sit down and say get right to the nitty-gritty at least
once or twice and it’s completely dehumanizing so we want to reassure parents that we’re not
going to do that to the child again will help the caregiver understand their role in the child’s
treatment since this modified since this model emphasizes working together as a team so I’m not
just going to be educating you it’s not going to be a parallel thing where I go in and I work with
Johnny and then I tell you what I did and then I work with Johnny I’m going to work with Johnny
and then we’re going to discuss what Johnny and I did in session and I’m going to get input from
you and we’re going to talk about how you feel about it and then I’m going to provide you with tools
so you can help Johnny outside of the session because you’re going to be with them for six-and-a-half
other days that I’m not and this can’t work if it’s just one hour once a week and we want to
elicit parent input questions and suggestions as much as possible because they’ve been living with
their kid for you know however many years so they probably have an idea about what works and what
doesn’t so we’ll start with both parents and children in their respective sessions helping
them understand what control breathing is and how it helps slow the heart rate and trigger the
wrist and digest sort of reaction in your body when your breathing slows your heart naturally
slows because the stress reaction tells your brain you’ve got to breathe fast and the heart
rates got to go fast well when you override that then you’re kind of overriding the whole system
and we’ll also talk about thought stopping and this is especially helpful if the trauma is recent
or and/or ever-present in the mind of the youth so they can say I am NOT going to talk about that right
now I’m not going to think about that right talk about distraction techniques go back to
your DBT stuff talks about improving the moment and accepts to help the child develop skills to
handle and work through when those thoughts pop up replace unthawed unwanted thoughts with
a pleasant one so talk about it in session when thoughts like that come up what would you
prefer to think about and then really get into the Nitty Gritty the five senses what do you see
smell hear taste you know help me get into that situation or that thought this teaches that
thoughts even unexpected and intrusive ones can be controlled so that gives them hope and again we’re
not exacerbating the thoughts right now we’re not bringing up their particular trauma and
having them get into detail we are just helping them deal with what’s happening normally on a
day-to-day basis so they feel like they have more control for the older kids you can have them
people log about when this technique is used what they were thinking about and how effective the
thought stopping was and then review it and help them tune it up if it’s not really effective and
give them praise for when they use it effectively relaxation training persons of Asian or Hispanic
origin tend to express stress in more somatic or physical terms so just be aware of that but that
doesn’t mean that Caucasians don’t relaxation training is good for anyone and the medical
school of South Carolina training recommended that relaxation is stress-free and
workbook by Davis Schulman and McKay so and it is still in publication when deciding how to
present relaxation techniques are creative have the child help you to integrate the elements
into the technique that makes it more relevant to them so, what are you thinking about when you
relax you know I know I like to go to the woods but maybe this kid likes to think about a video
game or play with their dog whatever it is but helps them make it relevant to them and then have
they identify other things they do to relax like drawing listening to music walking and making a
list of those things so they can refer to it when you’re teaching relaxation training especially if
you’re doing something like progressive muscular relaxation be sensitive to the child’s wishes if
they don’t wish to close their eyes or lie down which could trigger memories of the trauma we’re
not going there yet so if they feel vulnerable lying down or taking orders like that because
you can imagine how being told to lie down and close their eyes might be a trigger for certain
abuse survivors you know be cognizant of that and say you know get into a comfortable position
or how where would you like to sit while we talk about this like I said parents can often
benefit from the relaxation training as well so because they’re dealing with their issues
about the trauma but they’re also dealing with trying to figure out how to help Johnny and any
of them deal with any of Johnny’s misbehaviors or problematic behaviors then they move on to
feelings identification so it helps the therapist judge the child’s ability to articulate feelings
if you can tell me what makes you happy that’s great but if you can’t then you know we need to
work on figuring out what makes you happy you also want to help the child rate the intensity
of the emotion don’t let them stick with happy mad sad glad and afraid you know let’s talk about
different emotions and use the emotion chart with little faces on it or you can use the emotion
thermometer so is it a hot emotion or is it a cool emotion and helps the child
learn how to express feelings appropriately in different situations I mean sometimes they’re
going to be angry but it might not be appropriate to you know get up and stomp out of the room or
whatever however they communicate it so help them figure out how to articulate that so they can be
heard and supported some children have difficulty discussing or identifying their feelings so
you might try stepping back and discussing the feelings of other children or characters from
books or stories so you know think about Puff the Magic Dragon if they’ve read that you know
that dates me a little bit there but you know how did the little boy feel and talking about things
different characters and different stories where there are elements of anger and shame and loss and
all of that stuff helps children identify how they experience emotions if they seem detached
from the experience because sometimes they just they’ve shut it off it was just too overwhelming
so we want to talk about you know when you’re happy what does that feel like or when you’re
angry what happens what does your body feel like when you’re angry and they might be able
to tell you they hear their heartbeat in their ears or everything gets all fuzzy or whatever
but help them start tuning in to how they react and connecting that with an emotional word and then
after all, that’s done they can identify feelings they can identify feeling intensity now we want to
differentiate between thoughts and feelings many children describe thoughts when they’ve been
asked about a feeling so if you ask them how they feel they may say I want to run away so
you want to say okay well I hear that you want to run away so I’m wondering if you are bored and you
you’re bored and want to get away from it or if you’re scared can you tell me a little bit more
about what it means to you to want to run away during feelings identification the parent
sessions normalize what is going on with their child and help the parent understand that some
children may be seemingly in constant distress or detached from the trauma and that’s okay
we all react differently to traumas so again we’re going to share with the parents what we’re
Do let them know any specific difficulties if any juniors have encouraged the parent to praise
the child for appropriate management of difficult motions and I put in parenthesis successive
approximations because they’re not going to get it a hundred percent right every time so if they
try to effectively manage their emotions even a little bit let’s give them praise for that and
then help them figure out how to do it a little bit better the next time so instead of having a
complete meltdown maybe they got up and stomped out of the room well that’s an improvement so
then we want to talk about how to shape that behavior so it’s a more appropriate communication
if parents have difficulty identifying their own emotions provide them with examples so
continually ask them questions about how you feel when it’s a rainy day outside and how to do you
feel when somebody’s supposed to call you and they don’t how do you feel when and have about 15 or 20
examples and you can have them on a piece of paper and even give it to the parent to take home for
their homework if parents are overcome with their own emotions about the trauma validate
their feelings and explain how children need to see that their parents can handle talking
about the trauma so there the children need to see the strength and the parents which is what you’re
going to work on in parent sessions to make sure that the parents have the resolve and the skills
handle talking about this topic with junior TFC BT can be an effective intervention
for children or adolescents whose primary presenting issue is trauma-related emotional or
behavioral dysregulation TF CBT is not appropriate for clients who are actively suicidal and severely
depressed or currently abusing substances we want to make sure they’re clean
and sober as much as possible TF CBT starts with psychoeducation and then teaches stress
management and coping skills to aid in the management of distressing feelings psycho IDI
helps to clarify the inappropriate information children may have and start getting them a little
a bit more comfortable talking about the topic in general before we start going deeper and
feelings identification helps participants start effectively labeling and communicating their
feelings so they can receive the support and nurturance they need from their caregivers
and their support system if you enjoy this podcast please like and subscribe either in your
podcast player or on YouTube you can attend and participate in our live webinars with dr. Snipes
by subscribing to all CEUs comm slash counselor toolbox this episode has been brought to you in
part by all CEUs calm providing 24/7 multimedia continuing education and pre-certification
training to counselors therapists and nurses since 2006 use coupon code consular toolbox to
get a 20% discount on your order this month.
Etc sometimes you need to
delay joint sessions until the parent or caregiver can offer the child support and sometimes that
means not even starting treatment really until the parent and caregiver parent or caregiver
can be on board now you can get started with psychoeducation emotions identification feelings
identification and stress management and coping skills you know there were not really
poking a bunch of bears so you can probably safely get started on that if it’s sometimes it’s
court-ordered and they have to start treatment by April 1st or something so there are things you can
do but you may need to delay the actual beginning of the trauma narrative until the parent is
able to be available to educate everybody on how therapy works and instill in everyone not just
the parent optima optimist that well optimism about the child’s potential for recovery you
know sometimes they’ve been dealing with this child’s acting out behaviors for so long they’re
just like you know we’ve already been to three other therapists I don’t know what’s going to
fix it or I’ve done everything I know how to do good luck so we can talk about you know a
different approach or we can talk about what they’ve done that’s worked for a short period
of time and build on those strengths to instill optimism and hope and empowerment so
initially, when we talk about psycho-education it’s important to provide accurate information
about the trauma when children are traumatized they can be confused and not completely understand
what happened they may blame themselves and they may hold on to myths because they’ve been misled
and/or deliberately given incorrect information so one of the best ways we can help is to correct
that information provides information about how often this happens and whether you know it’s okay
to do this that or the other psychoeducation clarifies inappropriate information children may
have obtained directly from the perpetrator or on their own so the perpetrator may have told them
that this is how I express love or this is how you need to be disciplined because you don’t learn
this is how I was disciplined whatever it is or they could have gotten it on their own they could
have gotten it from school from the internet or just come up with it in their little heads trying
to make sense of what happened psychoeducation also helps them identify safety issues the
difference between safe situations and dangerous situations and as we get through this I really
want you to get away from the notion that TF CBT and childhood trauma are only physical and sexual
abuse there are so many other traumas as evidenced by the adverse childhood experiences survey that
I want you to wrap your head around that and there are things they didn’t cover in the aces such as
bullying and natural disasters so we want to help children whatever the trauma is the trauma made
they feel unsafe so we want to identify safety issues if the trauma was a hurricane then we want
to talk about what hurricanes are how often they hit what to safety plan etc so every time a
the thunderstorm comes they don’t freak out and we want to use psychoeducation to provide another
way to target faulty or maladaptive beliefs by helping to normalize thoughts and feelings about
the traumatic experience you know it makes sense that that was scary and makes sense that
you’re angry it makes sense that you feel this way and we can talk about why that makes
sense and why it makes you feel that way through cycle education you’re getting the child to start
talking about the specific trauma that he or she experienced in a less anxiety-provoking way by
talking in Jen wrong about the type of trauma so you’re talking about natural disasters you’re
talking about plane crashes you’re talking about domestic violence so they start learning about
it and then eventually you’re going to move down to their experience with it so like I said there
are a ton of different traumas and the ACE study even acknowledges that these are just the ten most
common ones that they heard however there are many many many different traumas and types of trauma
some of the biggest ones are physical and sexual abuse physical neglect emotional abuse
and neglect and the Aces identified mother treated violently I would say anyone in the household
treated violently it’s not just the mother’s substance misuse within the household and that
can be by the parents or by siblings household mental illness parental separation or divorce and
an incarcerated household member so those were aces but then like I said there’s also bullying
the death of a parent or sibling is extremely traumatic hurricane tornado natural disaster and
then I put the fire out separately because sometimes fire can be man-made sometimes it can be a wiring
problem but sometimes it can be Jr was playing with matches now even if jr. Accidentally started
the fire does that make it any less traumatic no it probably makes it more traumatic because then
there’s a whole sense of guilt and responsibility but it’s still a trauma that has to be dealt
with so I put a link to the adverse childhood experiences website if you want to go look more
about that but we’re going to move on psycho-education involves specific information about
the traumatic events the child has experienced not the child’s event we’re not going to go
into police records or something, we’re just going to talk about specific information about
domestic violence or whatever body awareness and sex education in cases of physical or sexual
maltreatment and there are caveats for getting parental consent and permission and all that other
stuff and Risk Reduction skills to decrease the risk of future traumatization now going back to
those other things it’s not just about physical or sexual abuse so we want to look at what was the
the risk created by you know how can you reduce your risk of being bullied how can you reduce your
risk of being traumatized in a tornado you know you can’t stop the tornado from coming
and they’re everywhere so what do you do and talk about a safety plan the same thing with fire
information needs to be tailored to fit a child’s particularly particular experiences and level
of knowledge obviously, you’re going to provide different information to a seven-year-old than
you are to a 17-year-old provide caregivers with handout materials to reinforce the information
discussed in session so this may help educate the parents about some of it but it lets them
know what you talked about and it gets us all on the literal same page you’re providing them a
handout of everything you went over with Junior and we want to encourage caregivers to discuss
this information at home reinforces accurate information about how safe or unsafe they
are and obviously, we’re going towards safe and reinforced accurate information and develop
a safety plan so they feel confident that at home they’re going to be taken care of when you
start psychoeducation you do want to get a sense of what the child already knows and you can use
a question-and-answer game format in which the child gets points for answering questions which I
love this suggestion so you can ask them if you know what is a hurricane or is a tornado and see
if they know and see if they know how much time and much-advanced warning we have for a tornado
versus a hurricane or you know whatever situation you’re talking about you see I did a lot of posts
Hurricane Katrina counseling in northern Florida so that’s one of those things that comes up for
I am talking with children about how likely is it that a category 5 hurricane is going to hit
again but encouraging them to give your aunt’s give answers and if they give the wrong answer you
know it’s great to try now you know try to coach them into a correct answer or provide them the correct
one but give them credit for at least making an effort sample questions might include what is
you know and put in the type of trauma what is bullying how often do you think bullying happens
and why does bullying happen you know those are some questions you can ask to just open a dialogue
about bullying, if this child has been a victim of bullying and is and is traumatized so cultural
considerations meet the child and family where they are by presenting information in a way which
they can relate it to their belief system and you may need to consult with their spiritual
guidance guides leaders whether it be a pastor or you know whatever to get some guidance
on how to handle certain aspects of whether it was the will of God and in the case of sexual abuse
how to handle the concept of virginity and how to handle the concept of bad things happening to bad
people and whatever else they think is coming from or their parents are instilling in them in a
belief system we want to make sure that we’re not necessarily contradicting it and going oh mom dad
and the church is wrong but we also want to help them try to integrate this in a way that can help
they have strong self-esteem so reaching out to those spiritual leaders and the family asking what
their belief system about certain things can be very helpful assess the general beliefs about
the trauma if something happened or when something happens ask the parent or the family that’s there
not necessarily the child but you want to get a sense of what the family stance is on why this
happened what it means how it’s going to impact life hence foreign henceforth and forever more
focus on the events they perceive as traumatic to the family but most especially the child if the
child’s going back to the Aces you know maybe the parents got divorced but the child doesn’t
see that as traumatic because there was domestic violence ahead of time the domestic violence was
traumatic the divorce was a relief so wherever the child is with each trauma we want to
be respectful of what they perceive is traumatic and tailor the information so the family can be
more receptive to it as supportive as possible and sometimes you need to make sure that the language
you know make sure the language is not jargony about general views of mental health and mental health
treatment should also be assessed and addressed in the psychoeducation piece not only with the child
but also with the family, if they are suspicious of it don’t understand it think that you’re just
going to magically fix Junior we want to demystify the process and talk about what is the purpose of
the assessment what is the purpose of each one of these activities and why am I doing this or why
are we doing this as a team and how can it help and then we also want to provide information to
D stigmatize and normalize mental health issues and seeking treatment some cultures are still
resistant to seeking treatment and I use the term cultures broadly because there’s
a stigma associated with it so normalizing for them how many people go to treatment how common
PTSD is or whatever the situation you’re dealing with it doesn’t mean they have to like it but at
At least it will give them a little bit of a nugget to understand that they’re not the only ones if
they are from a cultural group a minority cultural group of some sort you might want to provide
information about how common this particular issue is in their group I’ve done a lot of work
with law enforcement and emergency responders and they’re kind of their little group so
we talk about how common depression is among law enforcement and emergent emergency responders
specifically, because they face so much so many different stressors than you know Joe Schmo over
here so it D stigmatizes and normalizes a little bit now they still may not talk about it and
go well hey you know 37% of us have clinical depression no that’s probably not going to happen
but at least in the back of their mind, they can go you know what I’m looking around this room and
I can bet that at least one other person’s on antidepressants or something and feel a little
less unique and isolated in parent sessions you want to provide a rationale and overview of the
treatment model educates parents about the trauma and talks about the child’s trauma-related symptoms
so we’re going to go over what is hyper-vigilance what is the function it why people become
hypervigilant after trauma and what might it look like in a child because it presents very
differently for different children so we might want to give some ideas and say does this sound
like Johnny or does this sound like Johnny and help them understand why these behaviors may
be coming out we want to talk about how early treatment helps prevent long-term problems okay
maybe the trauma happened three years ago but still, it’s better than waiting ten more years and
you know Johnny’s still not having any Ellucian will want to talk about the importance of talking
directly about the trauma to help the children cope with their experiences and not hedging and
this will be on a case-by-case basis but the manual walks you through handling this discussion with
the parents about exactly how much detail do I go into if Johnny brings it up at home reassure
parents that children will first be taught skills to help them cope with their discomfort
and that talking about the trauma will be done slowly with a great deal of support so we’re not
just going to plop them down and go okay and tell me about the day that all this happened which
is what the child has experienced already if it was reported to law enforcement and/or the child
welfare they’ve probably had somebody sit down and say get right to the nitty-gritty at least
once or twice and it’s completely dehumanizing so we want to reassure parents that we’re not
going to do that to the child again will help the caregiver understand their role in the child’s
treatment since this modified since this model emphasizes working together as a team so I’m not
just going to be educating you it’s not going to be a parallel thing where I go in and I work with
Johnny and then I tell you what I did and then I work with Johnny I’m going to work with Johnny
and then we’re going to discuss what Johnny and I did in session and I’m going to get input from
you and we’re going to talk about how you feel about it and then I’m going to provide you with tools
so you can help Johnny outside of the session because you’re going to be with them for six-and-a-half
other days that I’m not and this can’t work if it’s just one hour once a week and we want to
elicit parent input questions and suggestions as much as possible because they’ve been living with
their kid for you know however many years so they probably have an idea about what works and what
doesn’t so we’ll start with both parents and children in their respective sessions helping
them understand what control breathing is and how it helps slow the heart rate and trigger the
wrist and digest sort of reaction in your body when your breathing slows your heart naturally
slows because the stress reaction tells your brain you’ve got to breathe fast and the heart
rates got to go fast well when you override that then you’re kind of overriding the whole system
and we’ll also talk about thought stopping and this is especially helpful if the trauma is recent
or and/or ever-present in the mind of the youth so they can say I am NOT going to talk about that right
now I’m not going to think about that right talk about distraction techniques go back to
your DBT stuff talks about improving the moment and accepts to help the child develop skills to
handle and work through when those thoughts pop up replace unthawed unwanted thoughts with
a pleasant one so talk about it in session when thoughts like that come up what would you
prefer to think about and then really get into the Nitty Gritty the five senses what do you see
smell hear taste you know help me get into that situation or that thought this teaches that
thoughts even unexpected and intrusive ones can be controlled so that gives them hope and again we’re
not exacerbating the thoughts right now we’re not bringing up their particular trauma and
having them get into detail we are just helping them deal with what’s happening normally on a
day-to-day basis so they feel like they have more control for the older kids you can have them
people log about when this technique is used what they were thinking about and how effective the
thought stopping was and then review it and help them tune it up if it’s not really effective and
give them praise for when they use it effectively relaxation training persons of Asian or Hispanic
origin tend to express stress in more somatic or physical terms so just be aware of that but that
doesn’t mean that Caucasians don’t relaxation training is good for anyone and the medical
school of South Carolina training recommended that relaxation is stress-free and
workbook by Davis Schulman and McKay so and it is still in publication when deciding how to
present relaxation techniques are creative have the child help you to integrate the elements
into the technique that makes it more relevant to them so, what are you thinking about when you
relax you know I know I like to go to the woods but maybe this kid likes to think about a video
game or play with their dog whatever it is but helps them make it relevant to them and then have
they identify other things they do to relax like drawing listening to music walking and making a
list of those things so they can refer to it when you’re teaching relaxation training especially if
you’re doing something like progressive muscular relaxation be sensitive to the child’s wishes if
they don’t wish to close their eyes or lie down which could trigger memories of the trauma we’re
not going there yet so if they feel vulnerable lying down or taking orders like that because
you can imagine how being told to lie down and close their eyes might be a trigger for certain
abuse survivors you know be cognizant of that and say you know get into a comfortable position
or how where would you like to sit while we talk about this like I said parents can often
benefit from the relaxation training as well so because they’re dealing with their issues
about the trauma but they’re also dealing with trying to figure out how to help Johnny and any
of them deal with any of Johnny’s misbehaviors or problematic behaviors then they move on to
feelings identification so it helps the therapist judge the child’s ability to articulate feelings
if you can tell me what makes you happy that’s great but if you can’t then you know we need to
work on figuring out what makes you happy you also want to help the child rate the intensity
of the emotion don’t let them stick with happy mad sad glad and afraid you know let’s talk about
different emotions and use the emotion chart with little faces on it or you can use the emotion
thermometer so is it a hot emotion or is it a cool emotion and helps the child
learn how to express feelings appropriately in different situations I mean sometimes they’re
going to be angry but it might not be appropriate to you know get up and stomp out of the room or
whatever however they communicate it so help them figure out how to articulate that so they can be
heard and supported some children have difficulty discussing or identifying their feelings so
you might try stepping back and discussing the feelings of other children or characters from
books or stories so you know think about Puff the Magic Dragon if they’ve read that you know
that dates me a little bit there but you know how did the little boy feel and talking about things
different characters and different stories where there are elements of anger and shame and loss and
all of that stuff helps children identify how they experience emotions if they seem detached
from the experience because sometimes they just they’ve shut it off it was just too overwhelming
so we want to talk about you know when you’re happy what does that feel like or when you’re
angry what happens what does your body feel like when you’re angry and they might be able
to tell you they hear their heartbeat in their ears or everything gets all fuzzy or whatever
but help them start tuning in to how they react and connecting that with an emotional word and then
after all, that’s done they can identify feelings they can identify feeling intensity now we want to
differentiate between thoughts and feelings many children describe thoughts when they’ve been
asked about a feeling so if you ask them how they feel they may say I want to run away so
you want to say okay well I hear that you want to run away so I’m wondering if you are bored and you
you’re bored and want to get away from it or if you’re scared can you tell me a little bit more
about what it means to you to want to run away during feelings identification the parent
sessions normalize what is going on with their child and help the parent understand that some
children may be seemingly in constant distress or detached from the trauma and that’s okay
we all react differently to traumas so again we’re going to share with the parents what we’re
Do let them know any specific difficulties if any juniors have encouraged the parent to praise
the child for appropriate management of difficult motions and I put in parenthesis successive
approximations because they’re not going to get it a hundred percent right every time so if they
try to effectively manage their emotions even a little bit let’s give them praise for that and
then help them figure out how to do it a little bit better the next time so instead of having a
complete meltdown maybe they got up and stomped out of the room well that’s an improvement so
then we want to talk about how to shape that behavior so it’s a more appropriate communication
if parents have difficulty identifying their own emotions provide them with examples so
continually ask them questions about how you feel when it’s a rainy day outside and how to do you
feel when somebody’s supposed to call you and they don’t how do you feel when and have about 15 or 20
examples and you can have them on a piece of paper and even give it to the parent to take home for
their homework if parents are overcome with their own emotions about the trauma validate
their feelings and explain how children need to see that their parents can handle talking
about the trauma so there the children need to see the strength and the parents which is what you’re
going to work on in parent sessions to make sure that the parents have the resolve and the skills
handle talking about this topic with junior TFC BT can be an effective intervention
for children or adolescents whose primary presenting issue is trauma-related emotional or
behavioral dysregulation TF CBT is not appropriate for clients who are actively suicidal and severely
depressed or currently abusing substances we want to make sure they’re clean
and sober as much as possible TF CBT starts with psychoeducation and then teaches stress
management and coping skills to aid in the management of distressing feelings psycho IDI
helps to clarify the inappropriate information children may have and start getting them a little
a bit more comfortable talking about the topic in general before we start going deeper and
feelings identification helps participants start effectively labeling and communicating their
feelings so they can receive the support and nurturance they need from their caregivers
and their support system if you enjoy this podcast please like and subscribe either in your
podcast player or on YouTube you can attend and participate in our live webinars with dr. Snipes
by subscribing to all CEUs comm slash counselor toolbox this episode has been brought to you in
part by all CEUs calm providing 24/7 multimedia continuing education and pre-certification
training to counselors therapists and nurses since 2006 use coupon code consular toolbox to
get a 20% discount on your order this month.