Unlimited CEUs for $59 are available at AllCEUs.com/Trauma-CEU this episode was pre-recorded
as part of a live continuing education webinar. CEUs are
still available at AllCEUs.com/Trauma-CEU welcome to today’s presentation on the
neurobiological impact of psychological trauma on the HPA axis we’re going to define and explain
the HPA axis which we’ve talked about before is a response system so it’s not
anything to get to you know overly concerned about that it’s going to be super dry well identify the
impact of trauma on this axis and on basically your whole nervous system in your brain identify
the impact of chronic stress and cumulative trauma on the HPA axis because a lot of times when
we talk about PTSD we think only about some particular acute event and that’s not necessarily
true there are a lot of people with PTSD who have basically what I call cumulative trauma and they
were exposed to extensive child neglect they were in domestically violent relationships they were
in a situation where they were exposed to trauma over and above what a normal person would think lawfully think of law enforcement military personnel think first responders I mean
they see stuff that no human should have to see and they see it not only once but you know once
a week or once a month depending on kind of where you are so it’s important to understand well
one thing may not be so traumatic to create post-traumatic stress we’re going to look at some
of the reasons that PTSD symptoms may develop as a cumulative sort of thing which I found this
to be interesting anyway we’ll identify symptoms of dysfunction and we’ll talk about some
interventions that are useful for this population now my guess is none of you are prescribing
physicians so when we’re going through this you’re going to be going yeah that’s all well and good
what’s the exact point of thinking about exactly what this information is telling
me on each slide show used to be the hat to help my clients who have been annoyed by trauma and
have not yet developed any sort of PTSD symptoms or who have PTSD symptoms and how can I use this
information to better tailor my treatment plan to help them become more effective in managing their
symptoms this is kind of a unique presentation because it was based on only one article this
was a meta-analysis so it’s a long article and it’s a really good article that I would
strongly suggest looking at it in your resources section in the class it lays out the many changes
and/or conditions that are seamed in the brain and nervous system of people with PTSD so they really
looked at a lot of research longitudinally to see what we know and what we don’t know as clinicians
awareness that these changes can help us educate patients about their symptoms why do you feel this
way and find ways of adapting to improve quality of life so neurobiological abnormalities in PTSD
overlap with features found in traumatic brain injury so that started making a lot of researchers
go hmm you know traumatic brain injury there is something or again of course hurting part of
the brain so why are the symptoms similar in PTSD you’re going to find out pretty
soon is that PTSD does cause damage actual physical damage in the brain the response
of an individual to trauma depends not only on the stressor characteristics but also on factors
specific to the individual so somebody can see a trauma and not be as traumatized if you will as
someone else and part of these factors and there was a study done by Pi Newson Nader back
I believe the early 80s looked at triage factors for PTSD and some of the factors that
they found why certain traumas may be more traumatic than certain people versus others have to do
with this particular trauma, you’re experiencing it close to one of your safe zones where you
live where you work somewhere where you’re not where you’re supposed to be feel safe and if
so then it’s probably going to be perceived as more traumatic now again think about the survival
capacity or the survival function of this behavior when your brain says this is supposed to be a safe
zone and it’s not so I need to respond in kind you’re trying to protect yourself make sense the
similarity to the victim if it could happen to her if it could happen to him they’re like me it could
happen to me that makes me feel scared because we like to categorize the world in terms of using them
bad things happen to those people not to us people but if you’re looking at a victim who’s liked you
and you say well I am and us people then you’re going to have more difficulty separating it and
feeling safe and going well that couldn’t happen to me and the degree of helplessness you know if
you saw something and you were just like there was nothing I could do there’s a greater sense of
helplessness and horror then if you didn’t have that necessarily that same experience so those
are a couple of things as far as the prestress or perception that we want to consider when we’re
talking to our patients even if you’re not a therapist that works with the trauma specifically
some people refer out for that some people are working with an EMDR therapist and you know cool
but as important to understand and if you happen to go down this road with your clients help them
understand why they perceived that particular stressor so intensely versus some other stressor
that they think may have good English there oh well sorry they think should have stretched
them out more so their perception of the stressor prior traumatic experiences and we’re going to
learn that prior traumas do cause changes in the brain to prepare you basically
Therese bond more quickly when there’s a threat so prior traumatic experiences can send you from
zero to 100 a lot faster which means it’s going to be or could be more traumatic the amount of
stress in the preceding months if you’re already worn down and your body has already said I can’t
fight anymore it’s not doing any good then when it encounters PTSD and when it encounters a
trauma the body might be going I just can’t take another thing please just I can’t do it which
is why we see in people with PTSD chronic stress burnout and chronic fatigue this inability to
tolerate stress because the body’s just already waived them that white flag going I can’t do it
current mental health or addiction issues again that’s your body’s way of saying something in
the neurotransmitter something in the system is a little bit wonky and that means I’m not
going to be able to respond a hundred percent healthy and functionally to whatever’s going
on and the availability of social support now a lot of the research especially with emergency
service personnel points to the availability of social support within 24 hours of the trauma
so when there’s an officer-involved shooting when there’s something that they encounter on
the duty that’s trauma the ability to have social support within that first 24 hours preferably first
two-hour period to at least touch base with a social positive social support is vital to
helping somebody process the memories instead of just kind of them disappearing into never-never
land and getting solidified in an unhelpful way for the vast majority of the population though
psychological trauma is limited to an acute transient disturbance you see something that’s
traumatic you’re like oh my gosh Wow it is devastating and yeah is going to affect you for
a little while but in a week or two you’re kind of feeling like you got your land legs again so
there’s this subpopulation of the population there’s a small group that ends up developing
PTSD the signs and symptoms of PTSD reflect a persistent adaptation of the neurobiological
symptoms to witnessed trauma and I crossed out abnormal in the article it says abnormal and
I look at it as a perfectly normal adaptation because the body is either going with the reserves
I have right now I can’t deal or you know whatever it’s doing it’s trying to protect itself now it
may not be helpful but from a survival perspective it generally makes sense so I try
when I’m working with clients to help them see the functional nature of their symptoms
given the knowledge they had or the state they were in at the time so now to the HPA axis the
The hypothalamic-pituitary-adrenal axis aka your threat response system controls reactions
to stress and regulates many body processes including digestion the immune system mood and
emotions sexuality energy storage and expenditure so let’s think about this real quick when you’re
under stress, your body feels threatened I needs to survive so it sends out excitatory
neurotransmitters that get you wired up which kind of makes your digestion speed up
it can cause some cramping in the abdominal area your immune system is not really important
right now threat we’re not worried about the flu mood and emotions you tend to
be hyper-vigilant and more easily startled threat means fight or flee which means anger or anxiety
so you’ve got some stress emotions and I don’t want to say dysfunctional because they’re very
functional your body perceives a threat and it’s saying you need to do something sexually well if
there’s a threat this is no time to procreate so your body says let’s turn off those sex hormones
right now, because we need to use us for fighting and fleeing not procreating which is all well
and good but when we have reduced sex hormones it also reduces our serotonin availability which
serotonin is one of those calming chemicals which help us calm down the excitatory neurons
so without them, you stay revved up which brings us to energy storage and expenditure you’re
revved up you’re on high alert you’re staying up here and your body says you know what if
I’m going to survive this fight or flight I need fuel which means you need to eat preferably
high-fat high-sugar foods that give us instant energy and sustained energy we want calorie defense
stuff now thinking about it from that perspective you can see how when you’re under chronic stress
or a big stressor you know some of your symptoms make sense why do you want to go eat chocolate
or do whatever you do that’s my go-to pizza and chocolate when I’m stressed is generally what I
crave not what I need but what I crave so we want to help people understand that there’s a reason
it makes sense now we just have to figure out how to deal with it differently the ultimate
result of HPA axis activation is to increase levels of cortisol in the blood during times of
stress now cortisol is the hormone that goes out and sets off kind of this whole well there are
a couple before it but it sets off this whole event cortisol is your stress hormone cortisol
is the one who says no sex hormones right now you know and it monkeys with all your different
hormones to make sure and your energy storage to make sure that you’re ready for this fight or
flee its main role is to release glucose into the bloodstream in order to facilitate the fight
or flight now glucose is sugar is raising your blood sugar so you’ve got energy now we’re going
to talk regularly about glucocorticoids which are glucose hormones that make your body release
glucose which is mainly cortisol and that term is going to become important later I’m just
kind of throwing it out there right now cortisol also suppresses and modulates the immune system
digestive system and reproductive system so again cortisol is saying we’ve got this energy we’ve got
this threat let me figure out how to sort of dole out our resources right now for survival in the
now it’s cortisol is very present focused it’s not looking at you know the long-term and
going well this will pass cortisol is very right now HPA axis dysfunction the body reduces HPA axis
activation when it appears further fight-or-flight may not be beneficial and they call this hypo
cortisol ism so basically a threat response system is you know warning the alarm in
my dorm when I was in college used to have these really annoying blinking lights I because why I do
this all the time sorry the hypercritical ism is your body’s response to going if I keep fighting I
am just throwing good energy after bad there is no sense in surrendering so it turns down the system
and it stops producing as much cortisol that way it has cortisol your stress hormone for when there
is a bigger more threatening threat well what does that mean well we need cortisol is what
helps us get up in the morning our cortisol goes up and down throughout the day which helps us
have the energy to get up go to work do those sorts of things it’s a normal hormone when it’s
in the right balance hypo cortical cortisol ISM seen in stress-related disorders such as chronic
fatigue syndrome burnout and PTSD is actually a protective mechanism designed to conserve energy
during threats that are beyond the organism with us ability to cope so dysfunction in the axis
causes abnormal immune system activation so you have increased inflammation and allergic
reactions cortisol is also related to cortisone your body does not release its
natural antihistamines when you are pardon me under stress which is why your allergies seem to
bother you more which when your allergies bother you more you’re probably not sleeping as well at
night and we know that not sleeping as well at night keeps your HPA axis activated so you’re
fighting this battle you’re trying to squeeze blood out of a turnip basically because your body
said we’re not releasing any more cortisol I don’t care what you say but everything else you’re not
sleeping as well you’re still kind of revved up you’re fatigued and your body is going but there’s
a threat and back in your brain they’re going yep but it’s not a big enough threat yet so you can
see where this cascade you’re fighting inside your own body and all your systems are kind of arguing
irritable bowel syndrome such as constipation and diarrhea because cortisol speeds things up and if
you don’t have enough cortisol you know what might happen reduce tolerance to physical and mental
stresses including pain remember I said that sex hormones go down which means that the availability of
serotonin goes down we know that serotonin is not only involved somehow in mood it’s involved
with some level of anxiety reduction but we also know it’s involved in pain perception
so when serotonin goes down we perceive pain more acutely and altered levels of sex hormones
so fatigue and you’re like where did that come from well the HPA axis is activated see how
many times I can say that without tripping on my tongue when it’s activated it sends out these you
know excitatory neurotransmitters when you’re excited for too long you get fatigued
well interesting little caveat or thing here fatigue is actually an emotion generated in the
brain you know we’ve learned to label it which prevents damage to the body when the brain perceives
that further exertion could be harmful sounds similar to hypo cortisol ISM it is so what do
we know from athletes we know that fatigue and sports is largely independent of the state of
the muscles themselves so fatigued you know your muscles usually only work up to about 60% of
their ability to work and then fatigue starts to set in so there was still a big margin that you
could work before your muscles finally gave out and said hold no more I’ve got jelly legs but
your muscles quit you start feeling tired you start feeling exhausted so this is a protective
mechanism the body’s gone we need to conserve a little bit of energy because you have to get home
and shower and you know prepare to run in case the tiger chases you but what factors is your body
paying attention to but tells it OK whoa we need to stop so we’ve got enough reserve in the event
of a problem core temperature, you’re working out your core temperature goes up at a certain point
it goes that’s high enough your glycogen your blood sugar levels your oxygen levels in the brain
how thirsty you are whether you’re sleep-deprived, to begin with, it’s going to mean that you fatigue
a lot easier and the level of muscle soreness and fatigue going into that exercise session the
brain kind of takes all these factors into effect and goes okay I can unless you work out
this much and then I’m going to shut you down I’m wrong it’s off what they have found though
is we can override this so when clients come into our office, they’re fatigued they are they’re off
they’re just like I’m exhausted I’m agitated I’m irritable I’m not sleeping well I just uh okay so
with athletes, we know that psychological factors can be used to reduce fatigue such as their
emotional state if they go in in a positive emotional state or a hyped up energized emotional
state if they’re listening to really energizing music it can help them push past that fatigue
point a little bit if they know the endpoint maybe they know they’re doing three sets of ten
reps they’re going to push through faster or more effectively than if they’re working with the coach
and they have no idea how many sets they’ve got or how many reps they’ve got to do they’re just like
are you going to make a stop to other competitors that service motivation they’re looking around they’re
seeing other people doing it they’re going okay I got this and in the case of athletes visual
feedback you know they’re seeing growth in their muscles they’re seeing positive changes so they
can push through that fatigue a little bit more they’re like okay this is worth it so fatigue
is one sign that the body is getting ready to down-regulate that HPA axis and go conservation
in practice and counseling practice how can we help reduce mental fatigue and help clients
restore their age PA access functioning and one of the things I would challenge you to think
about is how can we increase their self-efficacy and their high ductless if you will in their
the emotional state that a can-do attitude increases their hardiness and resilience you know we talk
about those, a lot man make sure they know their endpoint where are they going what does their
what do their symptoms look like what is it going to look like in three weeks in three months
and what can we reasonably think will change you know let’s give them some tangible goals that
they can look at other competitors or motivational group therapy can be very helpful in dealing
with some of this stuff obviously, you’re not going to do a lot of trauma work in the group most of the
time but having other people around knowing that there are other people who are dealing with
PTSD and having support groups can be really helpful because they can cheer each other on and
go come on John you got this you just need to push I know this is a really tough week for you and
that can help people push through that fatigue and feedback now in the case of psychological
issues we’re not talking about visual feedback but we’re talking about looking at that treatment
plan or looking at their symptoms and being able to say you know what I have made progress I’m not
having nightmares as much as I actually slept through the night last night who knew and finding those
things that they can latch on to and go things are getting better you know they’re not going to get
exponentially better overnight likely but they are getting better and I can see this incremental
progress and in doing that we can help people get a sense increase that those dopamine levels
increase that learning and go okay I can do this we want to make sure that we are considering
their fatigue level though and not putting too much on them at once let’s look at really
small steps and then solidifying those steps not taking one step after another but taking one step
and then taking a breather for some of our clients helping them identify how they’re feeling and
be aware of their own fatigue level low cortisol has been found to relate to more severe PTSD
hyperarousal symptoms and you’re like yeah it took me quite a while to wrap my head around this
whole concept but it makes sense now so when you have low cortisol your body is conserving all
its energy can in case it needs to respond to an extreme threat the sensitized negative
feedback loop in veterans diagnosed with PTSD have they’ve shown that they’ve got greater ludic
corticoid responsiveness now remember I talked about cortisol being a glue to co-corticoids and
there’s just no nice way to talk about this without using really obnoxiously clinical
terms anyhow which means that the body is holding on and it’s going you’re not going to have cortisol
to just get irritable or happy or excited about just anything but if there’s a threat I’ll let you
have it unfortunately in patients with cortisol ISM when there’s a threat they have an exaggerated
response thank hyper-vigilance and I call it the flatter the Furious so their mood is either kind
of flat and they’re not really responsive too much but when there is something that startles them or
their body perceives as a threat all of a sudden their body dumps cortisol and dumps glucose into
the system which floods the system and if you’ve ever flooded your engine you know what happens
doesn’t respond quite as well but there are even more problems with this so evidence says that the
role of trauma experienced in sensitizing the HPA axis regulation is independent of PTSD development
okay so what does that mean that means even if somebody doesn’t develop PTSD clinical diagnosis
if they’ve had trauma HPA access is going to sensitize them a little bit and hold them back a little bit
more cortisol and be a little bit more reactive when there is trauma which means successive
traumas could produce success successively significant reactions in those with prior trauma
maybe more at risk of PTSD for later traumas so again as a clinician what does this mean for
me this means that if I’m working with a client who comes from a troubled childhood there were
adverse childhood events or you know whatever you want to label it they had chronic stress they
had trauma in their childhood even in the prenatal period they found I wanted to educate them about the
the fact that they are at a greater risk of developing PTSD if they’re exposed to more trauma so they
can learn how to keep their stress levels under control because it’s more important for
them according to this research because of some persistent brain changes that we’re going to see
core endocrine factors of PTSD include abnormal regulation of cortisol and thyroid hormones okay
so we’ve already talked about cortisol our stress hormone and you’re probably familiar with thyroid
hormones being sort of your metabolism hormone but what happens when cortisol goes down in the body
starting to rein in the energy thyroid hormones also go down hypo cortisol ism and PTSD occurs
due to increased negative feedback sensitivity of the HPA axis okay studies suggest that low
cortisol levels at the time of exposure to trauma may predict the development of PTSD so if their
cortisol levels were already low they were already suffering if you will from hypercortisolism and
remember we’ve seen hypercortisolism in burnout and you know regular old burnout chronic fatigue
syndrome as well as PTSD so we’re not just talking about veterans here if the cortisol levels are
already abnormally low and the body’s already started conserving cortisol when they’re
exposed to a trauma we can with more certainty predict which people are going to develop PTSD
symptoms back to those gluteal corticoids they interfere with the retrieval of traumatic memories
an effect that may independently prevent or reduce symptoms of PTSD so when cortisol is in
the system and it’s causing all the blood sugar to develop we’re not forming lots of
memories right now we’re just surviving which they hypothesize could prevent or reduce the symptoms
if those memories aren’t consolidated and they go away, or it could contribute to difficulty
in treating PTSD why well let’s think about it if people who’ve been exposed to trauma you
know hypercortisolism they respond to threats by increasing the amount of cortisol and political
corticoids exponentially have an exaggerated response than when they’re in our off and
we’re talking to them about their trauma, and they start to get upset they start to get excited there
the body’s going to start dumping all these gluten coke or turquoise and guess what it’s going to make it
more difficult for them to retrieve those memories potentially so it’s kind of an interesting thing
to look at because a lot of clients that I worked with PTSD have been like I can’t
remember why can I not remember and my very general response because they don’t want to know
about all this stuff generally is it’s your brain’s way of protecting you it’s your brain’s way of
saying there’s a threat right now and you need to protect yourself from the threat we don’t need
to be worrying about all those memories back there so we do some you know relaxation activities and
those sorts of things to help them you know get back down to baseline so we’re not continuing to
fight against those gluten Co corticoids and thus cortisol because when you fight with that what
happens the client generally gets progressively frustrated progressively upset and progressively
unable to think clearly and access those memories neurochemical factors corner or chemical
factors of PTSD include abnormal regulation of catecholamines serotonin amino acid peptide and
opioid neurotransmitters each of which is found in brain circuits that regulate and integrate the
stress and fear response now again if you’re thinking I’m never going to remember this for the
quiz don’t get too stressed out about it because I want you to take home the overarching concepts
I’m not going to ask you really nitpicky questions about stuff that you have absolutely no control
over or at least that’s what I tried to do that being said I want I think it’s important that you
know that all of these neurochemicals including opioids are involved in the regulation and
integration of stress and fear responses it’s not just serotonin or two dopamine the catecholamine
family including dopamine and norepinephrine are derived from the amino acid tyrosine now it’s
not really all that important but an interesting little aside is that norepinephrine is made from
the breakdown of dopamine so your focus and get up and go chemical is made from your pleasure
chemical interesting little concept there when a stressor is perceived the HPA axis releases
corticotropin-releasing hormone which interacts with norepinephrine to increase fear conditioning
and encoding of emotional memories enhance arousal and vigilant vigilance and increase endocrine
and autonomic responses to stress so when the threat response system is turned on it releases
cortisol which interacts with norepinephrine the stress hormone and they get up and go hormone
say there’s some really bad mojo brewing here which increases fear conditioning because the
heart rates go in and everything and the response is stress there’s an abundance of evidence
that norepinephrine accounts for certain classic aspects of PTSD including hyperarousal heightened
startle and increased encoding of fear memories so what about serotonin you know that’s supposed to
be one of our calming chemicals it where did it go poor serotonin transmission and PTSD
maybe may cause impulsivity hostility aggression depression and suicidality remember you’ve got
the downregulation of the sex hormones so less availability of serotonin and there are other
things that cause the serotonin to not be as available but they found that serotonin binding
to 5h t1a receptors and this is just a little soapbox I’m going to go on don’t differ between
patients with PTSD and controls so what does that tell us that’s the only way we can really
To figure out what’s going on in the brain in a live subject look at PET scans what we have figured
out or they’ve hypothesized is the fact that the serotonin may not transmit as effectively as it may
be a really weak connection it’s connecting but it’s you know it’s kind of like having a rabbit
ears you got to twist it to get the signal to come in correctly all right this is another one
just a concept I want you to think about all they’re looking at in the research is the 5-hit
1a receptor there are a ton of 5-ht serotonin 5-ht receptors and each one of these receptors is
involved in some aspect of addiction anxiety mood sexual behavior mood sleep so when we’re talking
about why SSRIs don’t work well SSRIs only bind to certain receptors and if we’re not picking
the right receptor if it is the serotonin at all then we’re probably barking up the wrong tree
I educate my patients about this if they decide they need to go on antidepressants just so they
don’t get frustrated as easily I mean it’s still frustrating but so they don’t feel hopeless if
the first medication they start taking doesn’t seem to work or makes it worse we talked about why
that might be because there are so many different receptors for each one of the neurotransmitters
there is a really cool table if you’re into this stuff it’s actually on Wikipedia and it talks
also about not only what these receptors do but also what chemicals and medicines act on
these receptors and how Food for Thought GABA has profound anxiolytic effects in part by
inhibiting the cortisol norepinephrine circuits so it turns down the excitatory circuits
patients with PTSD exhibit decreased peripheral benzodiazepine binding sites well we know that
when the body secretes a neurotransmitter goes to the other end and it binds like a lock-and-key
if you will or it knocks on the door and the door gets opened and it goes through however you want
to think about it basically what they found is in patients with PTSD the Kem GABA goes through
and the GABA levels are okay but then it knocks on the door to get let in or it tries to put its
key in the lock and there’s something wrong at the binding sites or the binding sites you know
somebody’s super glued them shut and they’re just not there which is why patients with PTSD tend
to have a harder time de-escalating when their anxiety and stuff gets up because the GABA is
there but it’s got no doors to go through no locks to bind with however you want to whatever
metaphor you want to use this may indicate the usefulness of emotion regulation and distress
tolerance skills due to the potential emotional dysregulation of these clients so remember we
talked about them having a more exaggerated get-up-and-go response to a perceived threat and
they also have a harder time calming down which is basically one of your primary tenants of emotional
dysregulation so one thing clinicians can do is help patients learn that okay their body
responds differently to stress than other people at least for right now so it’s important for
them to understand what emotional dysregulation is emotional regulation strategies as well as
distress tolerance skills to help them until they can calm down to baseline because it sometimes
takes them longer than other people as clinicians we also can help reduce excitotoxin in order to
reduce stress improve stress tolerance and enable the acquisition of new skills when the brain gets
really going when the cortisol is out there and the glucocorticoids are in there it’s actually
toxic and starts causing neurons to disappear which we’re going to talk about in a second it’s
kind of scary NMDA receptors have been implicated in synaptic plasticity.

Which means the brain’s
ability to adjust and adapt as well as learning and memory so these are good receptors I like
them glutamate binds with these receptors and high levels of glutamate are secreted during high
levels of stress glutamate remember is what GABA is made from but high levels of glutamate
it’s an excitatory neural net in the brain and overexposure of neurons to this glutamate can be
excited toxic and may contribute to the loss of neurons in the hippocampus of patients with PTSD
so we’re actually seeing brain volume decrease as a result of exposure to certain chemicals elevated
gluten core glucocorticoid and yeah glucocorticoids increases the sensitivity of these receptors so
you’ve got a bunch of glutamate being dumped and you’ve got a bunch of glucocorticoid you’ve got
cortisol in there making these receptors more sensitive so it’s got they’re more sensitive and
they’ve got more coming in which makes it a whole lot easier to become toxic and start causing
neuronal degradation what does that mean why do we care it may take clients with PTSD more time to
master new skills because of emotional reactivity but also because some of their synaptic plasticity
may be damaged so it may take them a little bit longer to actually acquire and integrate these
new skills it’s not saying they’re stupid they can remember it just fine however when they’re
an emotionally charged state and helping their brain learn that okay this isn’t a threat that’s one
of those sort of subconscious things that has to happen that can take longer if the brain becomes
excited toxic during stress inhibited learning and memory then it becomes excited toxic during
stress which inhibits learning and memory so it’s under stress things are excited toxic neurons
are starting to disappear so I’m wondering and I’m just hypothesizing here I don’t know the
answers obviously or I wouldn’t be practicing it but what happens during the exposure therapies
because that’s exactly what we’re doing is we are flooding the brain with all of these chemicals
and creating basically an excitotoxin now they found some evidence that exposure therapies can
be helpful according to the DOJ website but or not the DOJ I can’t even think of it right
now the VA website but you know I’m wondering long-term what the impact is endogenous opioids
natural painkillers act upon the same receptors activated by exogenous opioids like morphine and
heroin exerts an inhibitory influence on the HPA axis well we know that people take opiates
and it has depressant effects on them it slows them down and calms them down alterations in our
natural opioids may be involved in certain PTSD symptoms such as numbing stress-induced analgesia
and dissociation again think of any clients you’ve had who have been abused or even taken and not like
the side effects of opiates are what opiates do to some people make them feel more relaxed stress
induced and analgesia they don’t have as much physical pain sometimes they just it’s there
I don’t care pill another interesting factor is now truck zone which is used to oppose opiate
appears to be effective in treating symptoms of dissociation flashbacks in traumatized persons so
basically, they’re saying if we undo the endogenous opioids we can treat these symptoms it highlights
the risk of opiate abuse for persons with PTSD though because if endogenous opioids produce
some of these numbing symptoms and dissociative symptoms so they can get away from the pain and
the flashbacks then if they add to that you know oral opioids it could prove to be a very tempting
cocktail we do want to as clinicians figure out how we can assist them with their physical and
emotional distress tolerance so they don’t feel the need to numb and escape and you know I
can’t imagine what some people have seen have gone through and I’m not trying to take that away
from them, I’m trying to help them figure out how they can stay present and learn to integrate it
changes question marks in brain structure and one of the questions that’s come up in the research is
because there aren’t any longitudinal studies that looked at it was the hippocampal volume as low to
begin with which created a predisposition for PTSD or did PTSD create the smaller hippocampal volume
interesting hippocampus is implicated in the control of stress responses memory and contextual
aspects of fear conditioning so it helps you to find these triggers in the environment that
help you become aware with your senses about when there might be a trauma prolonged exposure
to stress and high levels of glucocorticoids damage the hippocampus we’ve talked about that
hippocampal volume reduction in PTSD may reflect the accumulated toxic effects of repeated exposure
to increased cortisol levels what I called earlier the flatter the Furious having you know your body
holding on to cortisol for this extreme stress and then when it perceives stress it’s either
nothing or it’s extreme there are no kind sort of mild stressors out there that decrease hippocampal
volumes might also be a pre-existing vulnerability factor for developing PTSD the amygdala yet
another brain structure is the Olympic structure involved in the emotional process and it’s
critical for the acquisition of fear responses functional imaging of studies has revealed hyper
responsiveness and PTSD during the presentation of stressful script cues or trauma reminders but
also patients show increased amygdala responses to general emotional stimuli that are not trauma
associated such as emotional faces so they show an increased responsivity to things they see on the
TV that aren’t trauma-related to people crying to people showing anger’s going to have a
stronger emotional amygdala response than people without PTSD so clients with PTSD may be more
emotionally responsive across the board leading to more emotional dysregulation again an area that
we can help provide them with tools for early adverse experiences including prenatal stress and stress
throughout childhood has profound and long-lasting effects on the development of neurobiological
symptoms the brain is developing and if is exposed to a lot of stress and some of these excited toxic
situations how does that differ in the amount of damage caused versus a brain that’s already kind
of pretty much-formed programming may change for subsequent stress reactivity and vulnerability
to develop PTSD so if these happen during childhood or at any time the brain can
basically reprogram and go that it’s a really dangerous place out there so I need to hold
on to cortisol and I need to hold on to these stress hormones because every time I turn around
it seems like there’s a threat so I am going to be hyper-vigilant and respond in an exaggerated way
to protect you from the outside world adult women with childhood trauma histories have been shown
to exhibit sensitization of both neuroendocrine and Audino stress responses so basically they’re
showing hypo cortisol ISM a variety of changes take place in the brains and nervous systems of
people with PTSD and we talked about a lot of those the key take-home point is stress can
actually get toxic in the brain and cause physical changes not just thought changes in the brain
preexisting issues causing hypo cortisol ism where the brain has already downregulated whether it’s
due to chronic illness or chronic psychological stress increases the likelihood of the development
of PTSD this points to the importance of prevention and early intervention of adverse
childhood experiences we really need to get in there and help these people develop distress
tolerance skills understanding of vulnerabilities so they’re not going from flat to furious all
the time and so that they can understand why their body kind of responds and why they respond
differently than others and you know as we talk about this and of course I’m regularly bringing up
DBT buzzwords if you will think about your clients if you’ve worked with any who’ve had borderline
personality disorder what kind of history do they have did they have just a great childhood no we
know that people with BPD generally had pretty chaotic childhoods so this research is also
kind of underscoring why they may react and act the way they do that flat to furious people with
hypo cortical ism may or may not have PTSD so we don’t want to say well you’re fine if you don’t
have PTSD symptoms we do know that every trauma potentially can cause the body to down-regulate
and I kind of look at it as conserving a little bit more of the energy that it needs each time so
instead of conserving 60% now it’s conserving 65 and 66 each time it encounters a stressor in order
to prepare for potential ongoing threats in the environment hypercortisolism sets the stage for
the flattened the furious leading to toxic levels of glutamate upon exposure to stressors which
can cause the theorized reduction in hippocampal volume and persistent negative brain changes now I
always say the brain can you know rebalance itself and all well that’s part of the plasticity that is
the really cool thing about our brain however as far as regenerating those neurons I haven’t found
any evidence in the research that we found a way to help people regenerate once we’ve already those
neurons are gone they’ve been killed off the brain has to find a workaround so it does take time
but I do believe people can minimize some of the impact of the trauma they may have experienced
people with PTSD are more reactive to emotional stimuli even stimuli unrelated to trauma again
think about some of your clients especially if you work in a residential situation where you’re
around on 24/7, you know for 30 or 60 days, and you may see some clients that seem to get upset
over everything and you’re like ah such a drama queen or such a drama king and to yourself not
to anybody else but when you think about it from this perspective it gives you a different
perspective and you might say oh maybe their body responds differently they’ve got more emotional
dysregulation because of prior trauma they’re not trying to overreact this is their body’s response
because it’s perceived threat so many times it gives me a different approach to working
with that client hypercortisolism results when the brain perceives that continued effort is futile
feelings of fatigue set in akin to reduced stress tolerance so think about you know when you’ve had
a really long stressful period you know weeks or months maybe you’re dealing with an ailing family
member or something it’s just a lot of stress and you start getting really tired and when you’re
really tired and you’re worn down and somebody gives you one more thing it’s that one more thing
normally wouldn’t bother you but right now you just can’t take it so we can see how there’s a
reduced stress tolerance when somebody’s already at this stage reducing fatigue in our clients can
be accomplished in part with psychological factors including motivation or knowledge of other people
who are dealing with similar things support groups feedback about their and making sure they have
frequent successes not once a week but I want to have them keep a journal every day of something
good that happened or something positive that may indicate they’re moving forward in their
treatment goals and knowledge of an endpoint.

Where are we going with this when is the treatment
going to end I don’t want most clients don’t want to be with us forever no matter how lovable
we are do you want to feel better and be done with us so having to help them see that there
is an endpoint we’re going to accomplish this goal this month and then we can reassess 46% of
people in the US are exposed to adverse childhood experiences so like I said this is a huge area
for early intervention where we can prevent people from developing PTSD later in life how awesome
would that be instruction and skills to handle emotional dysregulation including mindfulness
vulnerability prevention and awareness emotion regulation distress tolerance and problem-solving
could be wonderful additions to health curriculums anything any skills groups you do with children
or adolescents or even adults I mean just because they’re adults doesn’t mean that they’re safe
from PTSD or that they’ve crossed any threshold where they’re too old to learn we’re never too
old to learn of those exposed to trauma education about and normalization of their heightened
emotional reactivity and susceptibility to PTSD in the future may be helpful in increasing their
motivation for their current treatment protocol whatever it is but it also just normalizes things
so they don’t feel like they’re overreacting or they don’t feel guilty for being so tired
or whatever they’re experiencing right now are there any questions I know I went through
a lot of really complicated stuff but I thought it was really interesting not only the way
our brain reacts in order to protect us but how cross-cutting a lot of this stuff
was it not just PTSD we’re talking about necessarily but a lot of this information
applies to our clients with chronic fatigue burnout and chronic stress and we can
see that those people also are at risk at higher risk of PTSD should they be exposed
to trauma and none of us is immune I mean there are tornadoes there are hurricanes
there are you know things that happen that really stink so the more we can help clients
be aware of things develop skills and tools to prevent as much harm as possible I
think the more effective we are as clinicians depending on the client and I can do some
more research on the VA website because they’re really into medications for PTSD I
know ketamine which is a horse tranquilizer has been shown to be effective in people
with PTSD and there have been some others that have kind of given me pause ketamine
is a hypnotic you know most of the drugs they’re trying out right now are really in my
opinion they’re powerful drugs but a lot of them all of them that I know of have
pretty high addictive potentials too so they make me nervous but you know when you’re
weighing the when you’re going from a harm reduction model that’s not necessarily not
necessarily such the be-all-end-all I guess that’s interesting that you use ketamine in the ER it’s definitely powerful effective stuff and like I said earlier some of the
stuff that some of my clients and some people have seen done experienced I couldn’t even
imagine and you know sometimes for them to actually survive we may need to look at some
of these more intense more powerful drugs PTSD and veteran trauma is not are not my focus
right now and yes marijuana is being experimented with or looked at used whatever however you want
to look at it for PTSD treatment with veterans there’s pretty much not a drug out there they
haven’t tried to throw at it to see well what will this do I believe they were even using
LSD experimentally for a little while too you the VA I mean if you’re interested in this
topic let me see if I could pull that down into here, we go to the National Center
for PTSD US Department of Veterans Affairs has a lot of information if you go for
professionals, it has a ton more information if you can get on get some of your SI CEUs on
demand they do have some free CEUs for PTSD here I’ve never taken any of them but what
I’ve looked at when I’ve looked at like the PowerPoints the presentations and stuff I’m
sure they’re good so if you’re you do focus a lot on PTSD and you can get on-demand CEUs
then this might be a place to get some good free ones aside from DBT are there any other
evidence-based practices for therapy that you’ve seen work best in combination with the
medications cognitive processing therapy when you’re working specifically with veterans
and there is a free course on that too and this one I have gone through
and it’s really awesome CPT dot must seed and here I’ll just put it
into that education and this is a free course oops and here’s the other one ah golly everyone and
embryo does have a lot of research effectiveness with people with PTSD too so yes I would
definitely encourage people to explore all options alrighty everybody I really
appreciate you coming today and sticking with me through this topic and I will see
you on Thursday if you have any questions please feel free to email me or you can
always also send it to support that all CEUs com either way I get it and otherwise I
will see you on Tuesday thanks a bunch if you enjoy this podcast please like and
subscribe either in your podcast player or on YouTube you can attend and participate
in our live webinars with Doctor Snipes by subscribing at all CEUs comm slash
counselor toolbox this episode has been brought to you in part by all CEUs
com providing 24/7 multimedia continuing education and pre-certification training to
counselors therapists and nurses since 2006 used coupon code consular toolbox to get
a 20% discount on your order this month
As found on YouTube15 Modules Of Intimate Video Training With
Dr. Joe Vitale – You’re getting simple and proven steps to unlock the Awakened Millionaire Mindset: giving you a path to MORE money, …

 Which means the brain’s
ability to adjust and adapt as well as learning and memory so these are good receptors I like
them glutamate binds with these receptors and high levels of glutamate are secreted during high
levels of stress glutamate remember is what GABA is made from but high levels of glutamate
it’s an excitatory neural net in the brain and overexposure of neurons to this glutamate can be
excited toxic and may contribute to the loss of neurons in the hippocampus of patients with PTSD
so we’re actually seeing brain volume decrease as a result of exposure to certain chemicals elevated
gluten core glucocorticoid and yeah glucocorticoids increases the sensitivity of these receptors so
you’ve got a bunch of glutamate being dumped and you’ve got a bunch of glucocorticoid you’ve got
cortisol in there making these receptors more sensitive so it’s got they’re more sensitive and
they’ve got more coming in which makes it a whole lot easier to become toxic and start causing
neuronal degradation what does that mean why do we care it may take clients with PTSD more time to
master new skills because of emotional reactivity but also because some of their synaptic plasticity
may be damaged so it may take them a little bit longer to actually acquire and integrate these
new skills it’s not saying they’re stupid they can remember it just fine however when they’re
an emotionally charged state and helping their brain learn that okay this isn’t a threat that’s one
of those sort of subconscious things that has to happen that can take longer if the brain becomes
excited toxic during stress inhibited learning and memory then it becomes excited toxic during
stress which inhibits learning and memory so it’s under stress things are excited toxic neurons
are starting to disappear so I’m wondering and I’m just hypothesizing here I don’t know the
answers obviously or I wouldn’t be practicing it but what happens during the exposure therapies
because that’s exactly what we’re doing is we are flooding the brain with all of these chemicals
and creating basically an excitotoxin now they found some evidence that exposure therapies can
be helpful according to the DOJ website but or not the DOJ I can’t even think of it right
now the VA website but you know I’m wondering long-term what the impact is endogenous opioids
natural painkillers act upon the same receptors activated by exogenous opioids like morphine and
heroin exerts an inhibitory influence on the HPA axis well we know that people take opiates
and it has depressant effects on them it slows them down and calms them down alterations in our
natural opioids may be involved in certain PTSD symptoms such as numbing stress-induced analgesia
and dissociation again think of any clients you’ve had who have been abused or even taken and not like
the side effects of opiates are what opiates do to some people make them feel more relaxed stress
induced and analgesia they don’t have as much physical pain sometimes they just it’s there
I don’t care pill another interesting factor is now truck zone which is used to oppose opiate
appears to be effective in treating symptoms of dissociation flashbacks in traumatized persons so
basically, they’re saying if we undo the endogenous opioids we can treat these symptoms it highlights
the risk of opiate abuse for persons with PTSD though because if endogenous opioids produce
some of these numbing symptoms and dissociative symptoms so they can get away from the pain and
the flashbacks then if they add to that you know oral opioids it could prove to be a very tempting
cocktail we do want to as clinicians figure out how we can assist them with their physical and
emotional distress tolerance so they don’t feel the need to numb and escape and you know I
can’t imagine what some people have seen have gone through and I’m not trying to take that away
from them, I’m trying to help them figure out how they can stay present and learn to integrate it
changes question marks in brain structure and one of the questions that’s come up in the research is
because there aren’t any longitudinal studies that looked at it was the hippocampal volume as low to
begin with which created a predisposition for PTSD or did PTSD create the smaller hippocampal volume
interesting hippocampus is implicated in the control of stress responses memory and contextual
aspects of fear conditioning so it helps you to find these triggers in the environment that
help you become aware with your senses about when there might be a trauma prolonged exposure
to stress and high levels of glucocorticoids damage the hippocampus we’ve talked about that
hippocampal volume reduction in PTSD may reflect the accumulated toxic effects of repeated exposure
to increased cortisol levels what I called earlier the flatter the Furious having you know your body
holding on to cortisol for this extreme stress and then when it perceives stress it’s either
nothing or it’s extreme there are no kind sort of mild stressors out there that decrease hippocampal
volumes might also be a pre-existing vulnerability factor for developing PTSD the amygdala yet
another brain structure is the Olympic structure involved in the emotional process and it’s
critical for the acquisition of fear responses functional imaging of studies has revealed hyper
responsiveness and PTSD during the presentation of stressful script cues or trauma reminders but
also patients show increased amygdala responses to general emotional stimuli that are not trauma
associated such as emotional faces so they show an increased responsivity to things they see on the
TV that aren’t trauma-related to people crying to people showing anger’s going to have a
stronger emotional amygdala response than people without PTSD so clients with PTSD may be more
emotionally responsive across the board leading to more emotional dysregulation again an area that
we can help provide them with tools for early adverse experiences including prenatal stress and stress
throughout childhood has profound and long-lasting effects on the development of neurobiological
symptoms the brain is developing and if is exposed to a lot of stress and some of these excited toxic
situations how does that differ in the amount of damage caused versus a brain that’s already kind
of pretty much-formed programming may change for subsequent stress reactivity and vulnerability
to develop PTSD so if these happen during childhood or at any time the brain can
basically reprogram and go that it’s a really dangerous place out there so I need to hold
on to cortisol and I need to hold on to these stress hormones because every time I turn around
it seems like there’s a threat so I am going to be hyper-vigilant and respond in an exaggerated way
to protect you from the outside world adult women with childhood trauma histories have been shown
to exhibit sensitization of both neuroendocrine and Audino stress responses so basically they’re
showing hypo cortisol ISM a variety of changes take place in the brains and nervous systems of
people with PTSD and we talked about a lot of those the key take-home point is stress can
actually get toxic in the brain and cause physical changes not just thought changes in the brain
preexisting issues causing hypo cortisol ism where the brain has already downregulated whether it’s
due to chronic illness or chronic psychological stress increases the likelihood of the development
of PTSD this points to the importance of prevention and early intervention of adverse
childhood experiences we really need to get in there and help these people develop distress
tolerance skills understanding of vulnerabilities so they’re not going from flat to furious all
the time and so that they can understand why their body kind of responds and why they respond
differently than others and you know as we talk about this and of course I’m regularly bringing up
DBT buzzwords if you will think about your clients if you’ve worked with any who’ve had borderline
personality disorder what kind of history do they have did they have just a great childhood no we
know that people with BPD generally had pretty chaotic childhoods so this research is also
kind of underscoring why they may react and act the way they do that flat to furious people with
hypo cortical ism may or may not have PTSD so we don’t want to say well you’re fine if you don’t
have PTSD symptoms we do know that every trauma potentially can cause the body to down-regulate
and I kind of look at it as conserving a little bit more of the energy that it needs each time so
instead of conserving 60% now it’s conserving 65 and 66 each time it encounters a stressor in order
to prepare for potential ongoing threats in the environment hypercortisolism sets the stage for
the flattened the furious leading to toxic levels of glutamate upon exposure to stressors which
can cause the theorized reduction in hippocampal volume and persistent negative brain changes now I
always say the brain can you know rebalance itself and all well that’s part of the plasticity that is
the really cool thing about our brain however as far as regenerating those neurons I haven’t found
any evidence in the research that we found a way to help people regenerate once we’ve already those
neurons are gone they’ve been killed off the brain has to find a workaround so it does take time
but I do believe people can minimize some of the impact of the trauma they may have experienced
people with PTSD are more reactive to emotional stimuli even stimuli unrelated to trauma again
think about some of your clients especially if you work in a residential situation where you’re
around on 24/7, you know for 30 or 60 days, and you may see some clients that seem to get upset
over everything and you’re like ah such a drama queen or such a drama king and to yourself not
to anybody else but when you think about it from this perspective it gives you a different
perspective and you might say oh maybe their body responds differently they’ve got more emotional
dysregulation because of prior trauma they’re not trying to overreact this is their body’s response
because it’s perceived threat so many times it gives me a different approach to working
with that client hypercortisolism results when the brain perceives that continued effort is futile
feelings of fatigue set in akin to reduced stress tolerance so think about you know when you’ve had
a really long stressful period you know weeks or months maybe you’re dealing with an ailing family
member or something it’s just a lot of stress and you start getting really tired and when you’re
really tired and you’re worn down and somebody gives you one more thing it’s that one more thing
normally wouldn’t bother you but right now you just can’t take it so we can see how there’s a
reduced stress tolerance when somebody’s already at this stage reducing fatigue in our clients can
be accomplished in part with psychological factors including motivation or knowledge of other people
who are dealing with similar things support groups feedback about their and making sure they have
frequent successes not once a week but I want to have them keep a journal every day of something
good that happened or something positive that may indicate they’re moving forward in their
treatment goals and knowledge of an endpoint.
Which means the brain’s
ability to adjust and adapt as well as learning and memory so these are good receptors I like
them glutamate binds with these receptors and high levels of glutamate are secreted during high
levels of stress glutamate remember is what GABA is made from but high levels of glutamate
it’s an excitatory neural net in the brain and overexposure of neurons to this glutamate can be
excited toxic and may contribute to the loss of neurons in the hippocampus of patients with PTSD
so we’re actually seeing brain volume decrease as a result of exposure to certain chemicals elevated
gluten core glucocorticoid and yeah glucocorticoids increases the sensitivity of these receptors so
you’ve got a bunch of glutamate being dumped and you’ve got a bunch of glucocorticoid you’ve got
cortisol in there making these receptors more sensitive so it’s got they’re more sensitive and
they’ve got more coming in which makes it a whole lot easier to become toxic and start causing
neuronal degradation what does that mean why do we care it may take clients with PTSD more time to
master new skills because of emotional reactivity but also because some of their synaptic plasticity
may be damaged so it may take them a little bit longer to actually acquire and integrate these
new skills it’s not saying they’re stupid they can remember it just fine however when they’re
an emotionally charged state and helping their brain learn that okay this isn’t a threat that’s one
of those sort of subconscious things that has to happen that can take longer if the brain becomes
excited toxic during stress inhibited learning and memory then it becomes excited toxic during
stress which inhibits learning and memory so it’s under stress things are excited toxic neurons
are starting to disappear so I’m wondering and I’m just hypothesizing here I don’t know the
answers obviously or I wouldn’t be practicing it but what happens during the exposure therapies
because that’s exactly what we’re doing is we are flooding the brain with all of these chemicals
and creating basically an excitotoxin now they found some evidence that exposure therapies can
be helpful according to the DOJ website but or not the DOJ I can’t even think of it right
now the VA website but you know I’m wondering long-term what the impact is endogenous opioids
natural painkillers act upon the same receptors activated by exogenous opioids like morphine and
heroin exerts an inhibitory influence on the HPA axis well we know that people take opiates
and it has depressant effects on them it slows them down and calms them down alterations in our
natural opioids may be involved in certain PTSD symptoms such as numbing stress-induced analgesia
and dissociation again think of any clients you’ve had who have been abused or even taken and not like
the side effects of opiates are what opiates do to some people make them feel more relaxed stress
induced and analgesia they don’t have as much physical pain sometimes they just it’s there
I don’t care pill another interesting factor is now truck zone which is used to oppose opiate
appears to be effective in treating symptoms of dissociation flashbacks in traumatized persons so
basically, they’re saying if we undo the endogenous opioids we can treat these symptoms it highlights
the risk of opiate abuse for persons with PTSD though because if endogenous opioids produce
some of these numbing symptoms and dissociative symptoms so they can get away from the pain and
the flashbacks then if they add to that you know oral opioids it could prove to be a very tempting
cocktail we do want to as clinicians figure out how we can assist them with their physical and
emotional distress tolerance so they don’t feel the need to numb and escape and you know I
can’t imagine what some people have seen have gone through and I’m not trying to take that away
from them, I’m trying to help them figure out how they can stay present and learn to integrate it
changes question marks in brain structure and one of the questions that’s come up in the research is
because there aren’t any longitudinal studies that looked at it was the hippocampal volume as low to
begin with which created a predisposition for PTSD or did PTSD create the smaller hippocampal volume
interesting hippocampus is implicated in the control of stress responses memory and contextual
aspects of fear conditioning so it helps you to find these triggers in the environment that
help you become aware with your senses about when there might be a trauma prolonged exposure
to stress and high levels of glucocorticoids damage the hippocampus we’ve talked about that
hippocampal volume reduction in PTSD may reflect the accumulated toxic effects of repeated exposure
to increased cortisol levels what I called earlier the flatter the Furious having you know your body
holding on to cortisol for this extreme stress and then when it perceives stress it’s either
nothing or it’s extreme there are no kind sort of mild stressors out there that decrease hippocampal
volumes might also be a pre-existing vulnerability factor for developing PTSD the amygdala yet
another brain structure is the Olympic structure involved in the emotional process and it’s
critical for the acquisition of fear responses functional imaging of studies has revealed hyper
responsiveness and PTSD during the presentation of stressful script cues or trauma reminders but
also patients show increased amygdala responses to general emotional stimuli that are not trauma
associated such as emotional faces so they show an increased responsivity to things they see on the
TV that aren’t trauma-related to people crying to people showing anger’s going to have a
stronger emotional amygdala response than people without PTSD so clients with PTSD may be more
emotionally responsive across the board leading to more emotional dysregulation again an area that
we can help provide them with tools for early adverse experiences including prenatal stress and stress
throughout childhood has profound and long-lasting effects on the development of neurobiological
symptoms the brain is developing and if is exposed to a lot of stress and some of these excited toxic
situations how does that differ in the amount of damage caused versus a brain that’s already kind
of pretty much-formed programming may change for subsequent stress reactivity and vulnerability
to develop PTSD so if these happen during childhood or at any time the brain can
basically reprogram and go that it’s a really dangerous place out there so I need to hold
on to cortisol and I need to hold on to these stress hormones because every time I turn around
it seems like there’s a threat so I am going to be hyper-vigilant and respond in an exaggerated way
to protect you from the outside world adult women with childhood trauma histories have been shown
to exhibit sensitization of both neuroendocrine and Audino stress responses so basically they’re
showing hypo cortisol ISM a variety of changes take place in the brains and nervous systems of
people with PTSD and we talked about a lot of those the key take-home point is stress can
actually get toxic in the brain and cause physical changes not just thought changes in the brain
preexisting issues causing hypo cortisol ism where the brain has already downregulated whether it’s
due to chronic illness or chronic psychological stress increases the likelihood of the development
of PTSD this points to the importance of prevention and early intervention of adverse
childhood experiences we really need to get in there and help these people develop distress
tolerance skills understanding of vulnerabilities so they’re not going from flat to furious all
the time and so that they can understand why their body kind of responds and why they respond
differently than others and you know as we talk about this and of course I’m regularly bringing up
DBT buzzwords if you will think about your clients if you’ve worked with any who’ve had borderline
personality disorder what kind of history do they have did they have just a great childhood no we
know that people with BPD generally had pretty chaotic childhoods so this research is also
kind of underscoring why they may react and act the way they do that flat to furious people with
hypo cortical ism may or may not have PTSD so we don’t want to say well you’re fine if you don’t
have PTSD symptoms we do know that every trauma potentially can cause the body to down-regulate
and I kind of look at it as conserving a little bit more of the energy that it needs each time so
instead of conserving 60% now it’s conserving 65 and 66 each time it encounters a stressor in order
to prepare for potential ongoing threats in the environment hypercortisolism sets the stage for
the flattened the furious leading to toxic levels of glutamate upon exposure to stressors which
can cause the theorized reduction in hippocampal volume and persistent negative brain changes now I
always say the brain can you know rebalance itself and all well that’s part of the plasticity that is
the really cool thing about our brain however as far as regenerating those neurons I haven’t found
any evidence in the research that we found a way to help people regenerate once we’ve already those
neurons are gone they’ve been killed off the brain has to find a workaround so it does take time
but I do believe people can minimize some of the impact of the trauma they may have experienced
people with PTSD are more reactive to emotional stimuli even stimuli unrelated to trauma again
think about some of your clients especially if you work in a residential situation where you’re
around on 24/7, you know for 30 or 60 days, and you may see some clients that seem to get upset
over everything and you’re like ah such a drama queen or such a drama king and to yourself not
to anybody else but when you think about it from this perspective it gives you a different
perspective and you might say oh maybe their body responds differently they’ve got more emotional
dysregulation because of prior trauma they’re not trying to overreact this is their body’s response
because it’s perceived threat so many times it gives me a different approach to working
with that client hypercortisolism results when the brain perceives that continued effort is futile
feelings of fatigue set in akin to reduced stress tolerance so think about you know when you’ve had
a really long stressful period you know weeks or months maybe you’re dealing with an ailing family
member or something it’s just a lot of stress and you start getting really tired and when you’re
really tired and you’re worn down and somebody gives you one more thing it’s that one more thing
normally wouldn’t bother you but right now you just can’t take it so we can see how there’s a
reduced stress tolerance when somebody’s already at this stage reducing fatigue in our clients can
be accomplished in part with psychological factors including motivation or knowledge of other people
who are dealing with similar things support groups feedback about their and making sure they have
frequent successes not once a week but I want to have them keep a journal every day of something
good that happened or something positive that may indicate they’re moving forward in their
treatment goals and knowledge of an endpoint. Where are we going with this when is the treatment
going to end I don’t want most clients don’t want to be with us forever no matter how lovable
we are do you want to feel better and be done with us so having to help them see that there
is an endpoint we’re going to accomplish this goal this month and then we can reassess 46% of
people in the US are exposed to adverse childhood experiences so like I said this is a huge area
for early intervention where we can prevent people from developing PTSD later in life how awesome
would that be instruction and skills to handle emotional dysregulation including mindfulness
vulnerability prevention and awareness emotion regulation distress tolerance and problem-solving
could be wonderful additions to health curriculums anything any skills groups you do with children
or adolescents or even adults I mean just because they’re adults doesn’t mean that they’re safe
from PTSD or that they’ve crossed any threshold where they’re too old to learn we’re never too
old to learn of those exposed to trauma education about and normalization of their heightened
emotional reactivity and susceptibility to PTSD in the future may be helpful in increasing their
motivation for their current treatment protocol whatever it is but it also just normalizes things
so they don’t feel like they’re overreacting or they don’t feel guilty for being so tired
or whatever they’re experiencing right now are there any questions I know I went through
a lot of really complicated stuff but I thought it was really interesting not only the way
our brain reacts in order to protect us but how cross-cutting a lot of this stuff
was it not just PTSD we’re talking about necessarily but a lot of this information
applies to our clients with chronic fatigue burnout and chronic stress and we can
see that those people also are at risk at higher risk of PTSD should they be exposed
to trauma and none of us is immune I mean there are tornadoes there are hurricanes
there are you know things that happen that really stink so the more we can help clients
be aware of things develop skills and tools to prevent as much harm as possible I
think the more effective we are as clinicians depending on the client and I can do some
more research on the VA website because they’re really into medications for PTSD I
know ketamine which is a horse tranquilizer has been shown to be effective in people
with PTSD and there have been some others that have kind of given me pause ketamine
is a hypnotic you know most of the drugs they’re trying out right now are really in my
opinion they’re powerful drugs but a lot of them all of them that I know of have
pretty high addictive potentials too so they make me nervous but you know when you’re
weighing the when you’re going from a harm reduction model that’s not necessarily not
necessarily such the be-all-end-all I guess that’s interesting that you use ketamine in the ER it’s definitely powerful effective stuff and like I said earlier some of the
stuff that some of my clients and some people have seen done experienced I couldn’t even
imagine and you know sometimes for them to actually survive we may need to look at some
of these more intense more powerful drugs PTSD and veteran trauma is not are not my focus
right now and yes marijuana is being experimented with or looked at used whatever however you want
to look at it for PTSD treatment with veterans there’s pretty much not a drug out there they
haven’t tried to throw at it to see well what will this do I believe they were even using
LSD experimentally for a little while too you the VA I mean if you’re interested in this
topic let me see if I could pull that down into here, we go to the National Center
for PTSD US Department of Veterans Affairs has a lot of information if you go for
professionals, it has a ton more information if you can get on get some of your SI CEUs on
demand they do have some free CEUs for PTSD here I’ve never taken any of them but what
I’ve looked at when I’ve looked at like the PowerPoints the presentations and stuff I’m
sure they’re good so if you’re you do focus a lot on PTSD and you can get on-demand CEUs
then this might be a place to get some good free ones aside from DBT are there any other
evidence-based practices for therapy that you’ve seen work best in combination with the
medications cognitive processing therapy when you’re working specifically with veterans
and there is a free course on that too and this one I have gone through
and it’s really awesome CPT dot must seed and here I’ll just put it
into that education and this is a free course oops and here’s the other one ah golly everyone and
embryo does have a lot of research effectiveness with people with PTSD too so yes I would
definitely encourage people to explore all options alrighty everybody I really
appreciate you coming today and sticking with me through this topic and I will see
you on Thursday if you have any questions please feel free to email me or you can
always also send it to support that all CEUs com either way I get it and otherwise I
will see you on Tuesday thanks a bunch if you enjoy this podcast please like and
subscribe either in your podcast player or on YouTube you can attend and participate
in our live webinars with Doctor Snipes by subscribing at all CEUs comm slash
counselor toolbox this episode has been brought to you in part by all CEUs
com providing 24/7 multimedia continuing education and pre-certification training to
counselors therapists and nurses since 2006 used coupon code consular toolbox to get
a 20% discount on your order this monthAs found on YouTube15 Modules Of Intimate Video Training With Dr. Joe Vitale – You’re getting simple and proven steps to unlock the Awakened Millionaire Mindset: giving you a path to MORE money, …
Where are we going with this when is the treatment
going to end I don’t want most clients don’t want to be with us forever no matter how lovable
we are do you want to feel better and be done with us so having to help them see that there
is an endpoint we’re going to accomplish this goal this month and then we can reassess 46% of
people in the US are exposed to adverse childhood experiences so like I said this is a huge area
for early intervention where we can prevent people from developing PTSD later in life how awesome
would that be instruction and skills to handle emotional dysregulation including mindfulness
vulnerability prevention and awareness emotion regulation distress tolerance and problem-solving
could be wonderful additions to health curriculums anything any skills groups you do with children
or adolescents or even adults I mean just because they’re adults doesn’t mean that they’re safe
from PTSD or that they’ve crossed any threshold where they’re too old to learn we’re never too
old to learn of those exposed to trauma education about and normalization of their heightened
emotional reactivity and susceptibility to PTSD in the future may be helpful in increasing their
motivation for their current treatment protocol whatever it is but it also just normalizes things
so they don’t feel like they’re overreacting or they don’t feel guilty for being so tired
or whatever they’re experiencing right now are there any questions I know I went through
a lot of really complicated stuff but I thought it was really interesting not only the way
our brain reacts in order to protect us but how cross-cutting a lot of this stuff
was it not just PTSD we’re talking about necessarily but a lot of this information
applies to our clients with chronic fatigue burnout and chronic stress and we can
see that those people also are at risk at higher risk of PTSD should they be exposed
to trauma and none of us is immune I mean there are tornadoes there are hurricanes
there are you know things that happen that really stink so the more we can help clients
be aware of things develop skills and tools to prevent as much harm as possible I
think the more effective we are as clinicians depending on the client and I can do some
more research on the VA website because they’re really into medications for PTSD I
know ketamine which is a horse tranquilizer has been shown to be effective in people
with PTSD and there have been some others that have kind of given me pause ketamine
is a hypnotic you know most of the drugs they’re trying out right now are really in my
opinion they’re powerful drugs but a lot of them all of them that I know of have
pretty high addictive potentials too so they make me nervous but you know when you’re
weighing the when you’re going from a harm reduction model that’s not necessarily not
necessarily such the be-all-end-all I guess that’s interesting that you use ketamine in the ER it’s definitely powerful effective stuff and like I said earlier some of the
stuff that some of my clients and some people have seen done experienced I couldn’t even
imagine and you know sometimes for them to actually survive we may need to look at some
of these more intense more powerful drugs PTSD and veteran trauma is not are not my focus
right now and yes marijuana is being experimented with or looked at used whatever however you want
to look at it for PTSD treatment with veterans there’s pretty much not a drug out there they
haven’t tried to throw at it to see well what will this do I believe they were even using
LSD experimentally for a little while too you the VA I mean if you’re interested in this
topic let me see if I could pull that down into here, we go to the National Center
for PTSD US Department of Veterans Affairs has a lot of information if you go for
professionals, it has a ton more information if you can get on get some of your SI CEUs on
demand they do have some free CEUs for PTSD here I’ve never taken any of them but what
I’ve looked at when I’ve looked at like the PowerPoints the presentations and stuff I’m
sure they’re good so if you’re you do focus a lot on PTSD and you can get on-demand CEUs
then this might be a place to get some good free ones aside from DBT are there any other
evidence-based practices for therapy that you’ve seen work best in combination with the
medications cognitive processing therapy when you’re working specifically with veterans
and there is a free course on that too and this one I have gone through
and it’s really awesome CPT dot must seed and here I’ll just put it
into that education and this is a free course oops and here’s the other one ah golly everyone and
embryo does have a lot of research effectiveness with people with PTSD too so yes I would
definitely encourage people to explore all options alrighty everybody I really
appreciate you coming today and sticking with me through this topic and I will see
you on Thursday if you have any questions please feel free to email me or you can
always also send it to support that all CEUs com either way I get it and otherwise I
will see you on Tuesday thanks a bunch if you enjoy this podcast please like and
subscribe either in your podcast player or on YouTube you can attend and participate
in our live webinars with Doctor Snipes by subscribing at all CEUs comm slash
counselor toolbox this episode has been brought to you in part by all CEUs
com providing 24/7 multimedia continuing education and pre-certification training to
counselors therapists and nurses since 2006 used coupon code consular toolbox to get
a 20% discount on your order this monthAs found on YouTube15 Modules Of Intimate Video Training With Dr. Joe Vitale – You’re getting simple and proven steps to unlock the Awakened Millionaire Mindset: giving you a path to MORE money, …
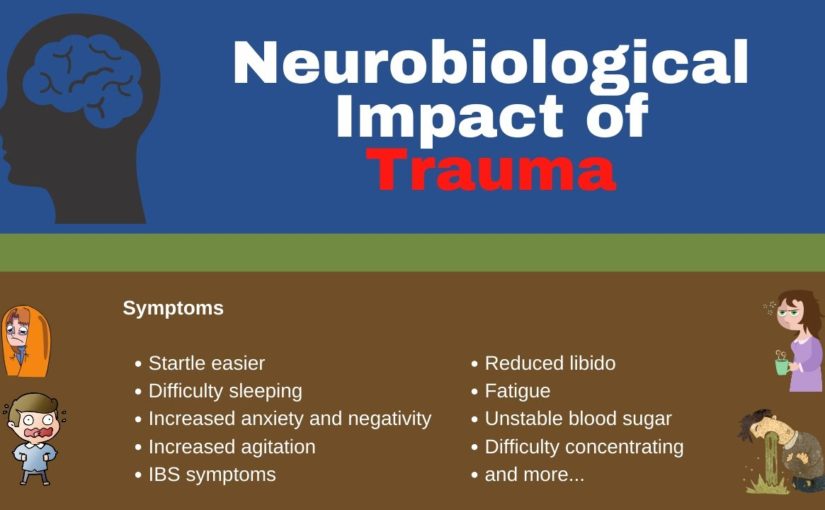

 Schneider by subscribing at all CEUs
calm / counselor toolbox this episode has been brought to you in part by all
CEUs calm providing 24/7 multimedia continuing education and pre
certification training to counselors therapists and nurses since 2006 use
coupon code consular toolbox to get a 20% discount off your order this month.
Schneider by subscribing at all CEUs
calm / counselor toolbox this episode has been brought to you in part by all
CEUs calm providing 24/7 multimedia continuing education and pre
certification training to counselors therapists and nurses since 2006 use
coupon code consular toolbox to get a 20% discount off your order this month.
 Etc sometimes you need to
delay joint sessions until the parent or caregiver can offer the child support and sometimes that
means not even starting treatment really until the parent and caregiver parent or caregiver
can be on board now you can get started with psychoeducation emotions identification feelings
identification and stress management and coping skills you know there were not really
poking a bunch of bears so you can probably safely get started on that if it’s sometimes it’s
court-ordered and they have to start treatment by April 1st or something so there are things you can
do but you may need to delay the actual beginning of the trauma narrative until the parent is
able to be available to educate everybody on how therapy works and instill in everyone not just
the parent optima optimist that well optimism about the child’s potential for recovery you
know sometimes they’ve been dealing with this child’s acting out behaviors for so long they’re
just like you know we’ve already been to three other therapists I don’t know what’s going to
fix it or I’ve done everything I know how to do good luck so we can talk about you know a
different approach or we can talk about what they’ve done that’s worked for a short period
of time and build on those strengths to instill optimism and hope and empowerment so
initially, when we talk about psycho-education it’s important to provide accurate information
about the trauma when children are traumatized they can be confused and not completely understand
what happened they may blame themselves and they may hold on to myths because they’ve been misled
and/or deliberately given incorrect information so one of the best ways we can help is to correct
that information provides information about how often this happens and whether you know it’s okay
to do this that or the other psychoeducation clarifies inappropriate information children may
have obtained directly from the perpetrator or on their own so the perpetrator may have told them
that this is how I express love or this is how you need to be disciplined because you don’t learn
this is how I was disciplined whatever it is or they could have gotten it on their own they could
have gotten it from school from the internet or just come up with it in their little heads trying
to make sense of what happened psychoeducation also helps them identify safety issues the
difference between safe situations and dangerous situations and as we get through this I really
want you to get away from the notion that TF CBT and childhood trauma are only physical and sexual
abuse there are so many other traumas as evidenced by the adverse childhood experiences survey that
I want you to wrap your head around that and there are things they didn’t cover in the aces such as
bullying and natural disasters so we want to help children whatever the trauma is the trauma made
they feel unsafe so we want to identify safety issues if the trauma was a hurricane then we want
to talk about what hurricanes are how often they hit what to safety plan etc so every time a
the thunderstorm comes they don’t freak out and we want to use psychoeducation to provide another
way to target faulty or maladaptive beliefs by helping to normalize thoughts and feelings about
the traumatic experience you know it makes sense that that was scary and makes sense that
you’re angry it makes sense that you feel this way and we can talk about why that makes
sense and why it makes you feel that way through cycle education you’re getting the child to start
talking about the specific trauma that he or she experienced in a less anxiety-provoking way by
talking in Jen wrong about the type of trauma so you’re talking about natural disasters you’re
talking about plane crashes you’re talking about domestic violence so they start learning about
it and then eventually you’re going to move down to their experience with it so like I said there
are a ton of different traumas and the ACE study even acknowledges that these are just the ten most
common ones that they heard however there are many many many different traumas and types of trauma
some of the biggest ones are physical and sexual abuse physical neglect emotional abuse
and neglect and the Aces identified mother treated violently I would say anyone in the household
treated violently it’s not just the mother’s substance misuse within the household and that
can be by the parents or by siblings household mental illness parental separation or divorce and
an incarcerated household member so those were aces but then like I said there’s also bullying
the death of a parent or sibling is extremely traumatic hurricane tornado natural disaster and
then I put the fire out separately because sometimes fire can be man-made sometimes it can be a wiring
problem but sometimes it can be Jr was playing with matches now even if jr. Accidentally started
the fire does that make it any less traumatic no it probably makes it more traumatic because then
there’s a whole sense of guilt and responsibility but it’s still a trauma that has to be dealt
with so I put a link to the adverse childhood experiences website if you want to go look more
about that but we’re going to move on psycho-education involves specific information about
the traumatic events the child has experienced not the child’s event we’re not going to go
into police records or something, we’re just going to talk about specific information about
domestic violence or whatever body awareness and sex education in cases of physical or sexual
maltreatment and there are caveats for getting parental consent and permission and all that other
stuff and Risk Reduction skills to decrease the risk of future traumatization now going back to
those other things it’s not just about physical or sexual abuse so we want to look at what was the
the risk created by you know how can you reduce your risk of being bullied how can you reduce your
risk of being traumatized in a tornado you know you can’t stop the tornado from coming
and they’re everywhere so what do you do and talk about a safety plan the same thing with fire
information needs to be tailored to fit a child’s particularly particular experiences and level
of knowledge obviously, you’re going to provide different information to a seven-year-old than
you are to a 17-year-old provide caregivers with handout materials to reinforce the information
discussed in session so this may help educate the parents about some of it but it lets them
know what you talked about and it gets us all on the literal same page you’re providing them a
handout of everything you went over with Junior and we want to encourage caregivers to discuss
this information at home reinforces accurate information about how safe or unsafe they
are and obviously, we’re going towards safe and reinforced accurate information and develop
a safety plan so they feel confident that at home they’re going to be taken care of when you
start psychoeducation you do want to get a sense of what the child already knows and you can use
a question-and-answer game format in which the child gets points for answering questions which I
love this suggestion so you can ask them if you know what is a hurricane or is a tornado and see
if they know and see if they know how much time and much-advanced warning we have for a tornado
versus a hurricane or you know whatever situation you’re talking about you see I did a lot of posts
Hurricane Katrina counseling in northern Florida so that’s one of those things that comes up for
I am talking with children about how likely is it that a category 5 hurricane is going to hit
again but encouraging them to give your aunt’s give answers and if they give the wrong answer you
know it’s great to try now you know try to coach them into a correct answer or provide them the correct
one but give them credit for at least making an effort sample questions might include what is
you know and put in the type of trauma what is bullying how often do you think bullying happens
and why does bullying happen you know those are some questions you can ask to just open a dialogue
about bullying, if this child has been a victim of bullying and is and is traumatized so cultural
considerations meet the child and family where they are by presenting information in a way which
they can relate it to their belief system and you may need to consult with their spiritual
guidance guides leaders whether it be a pastor or you know whatever to get some guidance
on how to handle certain aspects of whether it was the will of God and in the case of sexual abuse
how to handle the concept of virginity and how to handle the concept of bad things happening to bad
people and whatever else they think is coming from or their parents are instilling in them in a
belief system we want to make sure that we’re not necessarily contradicting it and going oh mom dad
and the church is wrong but we also want to help them try to integrate this in a way that can help
they have strong self-esteem so reaching out to those spiritual leaders and the family asking what
their belief system about certain things can be very helpful assess the general beliefs about
the trauma if something happened or when something happens ask the parent or the family that’s there
not necessarily the child but you want to get a sense of what the family stance is on why this
happened what it means how it’s going to impact life hence foreign henceforth and forever more
focus on the events they perceive as traumatic to the family but most especially the child if the
child’s going back to the Aces you know maybe the parents got divorced but the child doesn’t
see that as traumatic because there was domestic violence ahead of time the domestic violence was
traumatic the divorce was a relief so wherever the child is with each trauma we want to
be respectful of what they perceive is traumatic and tailor the information so the family can be
more receptive to it as supportive as possible and sometimes you need to make sure that the language
you know make sure the language is not jargony about general views of mental health and mental health
treatment should also be assessed and addressed in the psychoeducation piece not only with the child
but also with the family, if they are suspicious of it don’t understand it think that you’re just
going to magically fix Junior we want to demystify the process and talk about what is the purpose of
the assessment what is the purpose of each one of these activities and why am I doing this or why
are we doing this as a team and how can it help and then we also want to provide information to
D stigmatize and normalize mental health issues and seeking treatment some cultures are still
resistant to seeking treatment and I use the term cultures broadly because there’s
a stigma associated with it so normalizing for them how many people go to treatment how common
PTSD is or whatever the situation you’re dealing with it doesn’t mean they have to like it but at
At least it will give them a little bit of a nugget to understand that they’re not the only ones if
they are from a cultural group a minority cultural group of some sort you might want to provide
information about how common this particular issue is in their group I’ve done a lot of work
with law enforcement and emergency responders and they’re kind of their little group so
we talk about how common depression is among law enforcement and emergent emergency responders
specifically, because they face so much so many different stressors than you know Joe Schmo over
here so it D stigmatizes and normalizes a little bit now they still may not talk about it and
go well hey you know 37% of us have clinical depression no that’s probably not going to happen
but at least in the back of their mind, they can go you know what I’m looking around this room and
I can bet that at least one other person’s on antidepressants or something and feel a little
less unique and isolated in parent sessions you want to provide a rationale and overview of the
treatment model educates parents about the trauma and talks about the child’s trauma-related symptoms
so we’re going to go over what is hyper-vigilance what is the function it why people become
hypervigilant after trauma and what might it look like in a child because it presents very
differently for different children so we might want to give some ideas and say does this sound
like Johnny or does this sound like Johnny and help them understand why these behaviors may
be coming out we want to talk about how early treatment helps prevent long-term problems okay
maybe the trauma happened three years ago but still, it’s better than waiting ten more years and
you know Johnny’s still not having any Ellucian will want to talk about the importance of talking
directly about the trauma to help the children cope with their experiences and not hedging and
this will be on a case-by-case basis but the manual walks you through handling this discussion with
the parents about exactly how much detail do I go into if Johnny brings it up at home reassure
parents that children will first be taught skills to help them cope with their discomfort
and that talking about the trauma will be done slowly with a great deal of support so we’re not
just going to plop them down and go okay and tell me about the day that all this happened which
is what the child has experienced already if it was reported to law enforcement and/or the child
welfare they’ve probably had somebody sit down and say get right to the nitty-gritty at least
once or twice and it’s completely dehumanizing so we want to reassure parents that we’re not
going to do that to the child again will help the caregiver understand their role in the child’s
treatment since this modified since this model emphasizes working together as a team so I’m not
just going to be educating you it’s not going to be a parallel thing where I go in and I work with
Johnny and then I tell you what I did and then I work with Johnny I’m going to work with Johnny
and then we’re going to discuss what Johnny and I did in session and I’m going to get input from
you and we’re going to talk about how you feel about it and then I’m going to provide you with tools
so you can help Johnny outside of the session because you’re going to be with them for six-and-a-half
other days that I’m not and this can’t work if it’s just one hour once a week and we want to
elicit parent input questions and suggestions as much as possible because they’ve been living with
their kid for you know however many years so they probably have an idea about what works and what
doesn’t so we’ll start with both parents and children in their respective sessions helping
them understand what control breathing is and how it helps slow the heart rate and trigger the
wrist and digest sort of reaction in your body when your breathing slows your heart naturally
slows because the stress reaction tells your brain you’ve got to breathe fast and the heart
rates got to go fast well when you override that then you’re kind of overriding the whole system
and we’ll also talk about thought stopping and this is especially helpful if the trauma is recent
or and/or ever-present in the mind of the youth so they can say I am NOT going to talk about that right
now I’m not going to think about that right talk about distraction techniques go back to
your DBT stuff talks about improving the moment and accepts to help the child develop skills to
handle and work through when those thoughts pop up replace unthawed unwanted thoughts with
a pleasant one so talk about it in session when thoughts like that come up what would you
prefer to think about and then really get into the Nitty Gritty the five senses what do you see
smell hear taste you know help me get into that situation or that thought this teaches that
thoughts even unexpected and intrusive ones can be controlled so that gives them hope and again we’re
not exacerbating the thoughts right now we’re not bringing up their particular trauma and
having them get into detail we are just helping them deal with what’s happening normally on a
day-to-day basis so they feel like they have more control for the older kids you can have them
people log about when this technique is used what they were thinking about and how effective the
thought stopping was and then review it and help them tune it up if it’s not really effective and
give them praise for when they use it effectively relaxation training persons of Asian or Hispanic
origin tend to express stress in more somatic or physical terms so just be aware of that but that
doesn’t mean that Caucasians don’t relaxation training is good for anyone and the medical
school of South Carolina training recommended that relaxation is stress-free and
workbook by Davis Schulman and McKay so and it is still in publication when deciding how to
present relaxation techniques are creative have the child help you to integrate the elements
into the technique that makes it more relevant to them so, what are you thinking about when you
relax you know I know I like to go to the woods but maybe this kid likes to think about a video
game or play with their dog whatever it is but helps them make it relevant to them and then have
they identify other things they do to relax like drawing listening to music walking and making a
list of those things so they can refer to it when you’re teaching relaxation training especially if
you’re doing something like progressive muscular relaxation be sensitive to the child’s wishes if
they don’t wish to close their eyes or lie down which could trigger memories of the trauma we’re
not going there yet so if they feel vulnerable lying down or taking orders like that because
you can imagine how being told to lie down and close their eyes might be a trigger for certain
abuse survivors you know be cognizant of that and say you know get into a comfortable position
or how where would you like to sit while we talk about this like I said parents can often
benefit from the relaxation training as well so because they’re dealing with their issues
about the trauma but they’re also dealing with trying to figure out how to help Johnny and any
of them deal with any of Johnny’s misbehaviors or problematic behaviors then they move on to
feelings identification so it helps the therapist judge the child’s ability to articulate feelings
if you can tell me what makes you happy that’s great but if you can’t then you know we need to
work on figuring out what makes you happy you also want to help the child rate the intensity
of the emotion don’t let them stick with happy mad sad glad and afraid you know let’s talk about
different emotions and use the emotion chart with little faces on it or you can use the emotion
thermometer so is it a hot emotion or is it a cool emotion and helps the child
learn how to express feelings appropriately in different situations I mean sometimes they’re
going to be angry but it might not be appropriate to you know get up and stomp out of the room or
whatever however they communicate it so help them figure out how to articulate that so they can be
heard and supported some children have difficulty discussing or identifying their feelings so
you might try stepping back and discussing the feelings of other children or characters from
books or stories so you know think about Puff the Magic Dragon if they’ve read that you know
that dates me a little bit there but you know how did the little boy feel and talking about things
different characters and different stories where there are elements of anger and shame and loss and
all of that stuff helps children identify how they experience emotions if they seem detached
from the experience because sometimes they just they’ve shut it off it was just too overwhelming
so we want to talk about you know when you’re happy what does that feel like or when you’re
angry what happens what does your body feel like when you’re angry and they might be able
to tell you they hear their heartbeat in their ears or everything gets all fuzzy or whatever
but help them start tuning in to how they react and connecting that with an emotional word and then
after all, that’s done they can identify feelings they can identify feeling intensity now we want to
differentiate between thoughts and feelings many children describe thoughts when they’ve been
asked about a feeling so if you ask them how they feel they may say I want to run away so
you want to say okay well I hear that you want to run away so I’m wondering if you are bored and you
you’re bored and want to get away from it or if you’re scared can you tell me a little bit more
about what it means to you to want to run away during feelings identification the parent
sessions normalize what is going on with their child and help the parent understand that some
children may be seemingly in constant distress or detached from the trauma and that’s okay
we all react differently to traumas so again we’re going to share with the parents what we’re
Do let them know any specific difficulties if any juniors have encouraged the parent to praise
the child for appropriate management of difficult motions and I put in parenthesis successive
approximations because they’re not going to get it a hundred percent right every time so if they
try to effectively manage their emotions even a little bit let’s give them praise for that and
then help them figure out how to do it a little bit better the next time so instead of having a
complete meltdown maybe they got up and stomped out of the room well that’s an improvement so
then we want to talk about how to shape that behavior so it’s a more appropriate communication
if parents have difficulty identifying their own emotions provide them with examples so
continually ask them questions about how you feel when it’s a rainy day outside and how to do you
feel when somebody’s supposed to call you and they don’t how do you feel when and have about 15 or 20
examples and you can have them on a piece of paper and even give it to the parent to take home for
their homework if parents are overcome with their own emotions about the trauma validate
their feelings and explain how children need to see that their parents can handle talking
about the trauma so there the children need to see the strength and the parents which is what you’re
going to work on in parent sessions to make sure that the parents have the resolve and the skills
handle talking about this topic with junior TFC BT can be an effective intervention
for children or adolescents whose primary presenting issue is trauma-related emotional or
behavioral dysregulation TF CBT is not appropriate for clients who are actively suicidal and severely
depressed or currently abusing substances we want to make sure they’re clean
and sober as much as possible TF CBT starts with psychoeducation and then teaches stress
management and coping skills to aid in the management of distressing feelings psycho IDI
helps to clarify the inappropriate information children may have and start getting them a little
a bit more comfortable talking about the topic in general before we start going deeper and
feelings identification helps participants start effectively labeling and communicating their
feelings so they can receive the support and nurturance they need from their caregivers
and their support system if you enjoy this podcast please like and subscribe either in your
podcast player or on YouTube you can attend and participate in our live webinars with dr. Snipes
by subscribing to all CEUs comm slash counselor toolbox this episode has been brought to you in
part by all CEUs calm providing 24/7 multimedia continuing education and pre-certification
training to counselors therapists and nurses since 2006 use coupon code consular toolbox to
get a 20% discount on your order this month.
Etc sometimes you need to
delay joint sessions until the parent or caregiver can offer the child support and sometimes that
means not even starting treatment really until the parent and caregiver parent or caregiver
can be on board now you can get started with psychoeducation emotions identification feelings
identification and stress management and coping skills you know there were not really
poking a bunch of bears so you can probably safely get started on that if it’s sometimes it’s
court-ordered and they have to start treatment by April 1st or something so there are things you can
do but you may need to delay the actual beginning of the trauma narrative until the parent is
able to be available to educate everybody on how therapy works and instill in everyone not just
the parent optima optimist that well optimism about the child’s potential for recovery you
know sometimes they’ve been dealing with this child’s acting out behaviors for so long they’re
just like you know we’ve already been to three other therapists I don’t know what’s going to
fix it or I’ve done everything I know how to do good luck so we can talk about you know a
different approach or we can talk about what they’ve done that’s worked for a short period
of time and build on those strengths to instill optimism and hope and empowerment so
initially, when we talk about psycho-education it’s important to provide accurate information
about the trauma when children are traumatized they can be confused and not completely understand
what happened they may blame themselves and they may hold on to myths because they’ve been misled
and/or deliberately given incorrect information so one of the best ways we can help is to correct
that information provides information about how often this happens and whether you know it’s okay
to do this that or the other psychoeducation clarifies inappropriate information children may
have obtained directly from the perpetrator or on their own so the perpetrator may have told them
that this is how I express love or this is how you need to be disciplined because you don’t learn
this is how I was disciplined whatever it is or they could have gotten it on their own they could
have gotten it from school from the internet or just come up with it in their little heads trying
to make sense of what happened psychoeducation also helps them identify safety issues the
difference between safe situations and dangerous situations and as we get through this I really
want you to get away from the notion that TF CBT and childhood trauma are only physical and sexual
abuse there are so many other traumas as evidenced by the adverse childhood experiences survey that
I want you to wrap your head around that and there are things they didn’t cover in the aces such as
bullying and natural disasters so we want to help children whatever the trauma is the trauma made
they feel unsafe so we want to identify safety issues if the trauma was a hurricane then we want
to talk about what hurricanes are how often they hit what to safety plan etc so every time a
the thunderstorm comes they don’t freak out and we want to use psychoeducation to provide another
way to target faulty or maladaptive beliefs by helping to normalize thoughts and feelings about
the traumatic experience you know it makes sense that that was scary and makes sense that
you’re angry it makes sense that you feel this way and we can talk about why that makes
sense and why it makes you feel that way through cycle education you’re getting the child to start
talking about the specific trauma that he or she experienced in a less anxiety-provoking way by
talking in Jen wrong about the type of trauma so you’re talking about natural disasters you’re
talking about plane crashes you’re talking about domestic violence so they start learning about
it and then eventually you’re going to move down to their experience with it so like I said there
are a ton of different traumas and the ACE study even acknowledges that these are just the ten most
common ones that they heard however there are many many many different traumas and types of trauma
some of the biggest ones are physical and sexual abuse physical neglect emotional abuse
and neglect and the Aces identified mother treated violently I would say anyone in the household
treated violently it’s not just the mother’s substance misuse within the household and that
can be by the parents or by siblings household mental illness parental separation or divorce and
an incarcerated household member so those were aces but then like I said there’s also bullying
the death of a parent or sibling is extremely traumatic hurricane tornado natural disaster and
then I put the fire out separately because sometimes fire can be man-made sometimes it can be a wiring
problem but sometimes it can be Jr was playing with matches now even if jr. Accidentally started
the fire does that make it any less traumatic no it probably makes it more traumatic because then
there’s a whole sense of guilt and responsibility but it’s still a trauma that has to be dealt
with so I put a link to the adverse childhood experiences website if you want to go look more
about that but we’re going to move on psycho-education involves specific information about
the traumatic events the child has experienced not the child’s event we’re not going to go
into police records or something, we’re just going to talk about specific information about
domestic violence or whatever body awareness and sex education in cases of physical or sexual
maltreatment and there are caveats for getting parental consent and permission and all that other
stuff and Risk Reduction skills to decrease the risk of future traumatization now going back to
those other things it’s not just about physical or sexual abuse so we want to look at what was the
the risk created by you know how can you reduce your risk of being bullied how can you reduce your
risk of being traumatized in a tornado you know you can’t stop the tornado from coming
and they’re everywhere so what do you do and talk about a safety plan the same thing with fire
information needs to be tailored to fit a child’s particularly particular experiences and level
of knowledge obviously, you’re going to provide different information to a seven-year-old than
you are to a 17-year-old provide caregivers with handout materials to reinforce the information
discussed in session so this may help educate the parents about some of it but it lets them
know what you talked about and it gets us all on the literal same page you’re providing them a
handout of everything you went over with Junior and we want to encourage caregivers to discuss
this information at home reinforces accurate information about how safe or unsafe they
are and obviously, we’re going towards safe and reinforced accurate information and develop
a safety plan so they feel confident that at home they’re going to be taken care of when you
start psychoeducation you do want to get a sense of what the child already knows and you can use
a question-and-answer game format in which the child gets points for answering questions which I
love this suggestion so you can ask them if you know what is a hurricane or is a tornado and see
if they know and see if they know how much time and much-advanced warning we have for a tornado
versus a hurricane or you know whatever situation you’re talking about you see I did a lot of posts
Hurricane Katrina counseling in northern Florida so that’s one of those things that comes up for
I am talking with children about how likely is it that a category 5 hurricane is going to hit
again but encouraging them to give your aunt’s give answers and if they give the wrong answer you
know it’s great to try now you know try to coach them into a correct answer or provide them the correct
one but give them credit for at least making an effort sample questions might include what is
you know and put in the type of trauma what is bullying how often do you think bullying happens
and why does bullying happen you know those are some questions you can ask to just open a dialogue
about bullying, if this child has been a victim of bullying and is and is traumatized so cultural
considerations meet the child and family where they are by presenting information in a way which
they can relate it to their belief system and you may need to consult with their spiritual
guidance guides leaders whether it be a pastor or you know whatever to get some guidance
on how to handle certain aspects of whether it was the will of God and in the case of sexual abuse
how to handle the concept of virginity and how to handle the concept of bad things happening to bad
people and whatever else they think is coming from or their parents are instilling in them in a
belief system we want to make sure that we’re not necessarily contradicting it and going oh mom dad
and the church is wrong but we also want to help them try to integrate this in a way that can help
they have strong self-esteem so reaching out to those spiritual leaders and the family asking what
their belief system about certain things can be very helpful assess the general beliefs about
the trauma if something happened or when something happens ask the parent or the family that’s there
not necessarily the child but you want to get a sense of what the family stance is on why this
happened what it means how it’s going to impact life hence foreign henceforth and forever more
focus on the events they perceive as traumatic to the family but most especially the child if the
child’s going back to the Aces you know maybe the parents got divorced but the child doesn’t
see that as traumatic because there was domestic violence ahead of time the domestic violence was
traumatic the divorce was a relief so wherever the child is with each trauma we want to
be respectful of what they perceive is traumatic and tailor the information so the family can be
more receptive to it as supportive as possible and sometimes you need to make sure that the language
you know make sure the language is not jargony about general views of mental health and mental health
treatment should also be assessed and addressed in the psychoeducation piece not only with the child
but also with the family, if they are suspicious of it don’t understand it think that you’re just
going to magically fix Junior we want to demystify the process and talk about what is the purpose of
the assessment what is the purpose of each one of these activities and why am I doing this or why
are we doing this as a team and how can it help and then we also want to provide information to
D stigmatize and normalize mental health issues and seeking treatment some cultures are still
resistant to seeking treatment and I use the term cultures broadly because there’s
a stigma associated with it so normalizing for them how many people go to treatment how common
PTSD is or whatever the situation you’re dealing with it doesn’t mean they have to like it but at
At least it will give them a little bit of a nugget to understand that they’re not the only ones if
they are from a cultural group a minority cultural group of some sort you might want to provide
information about how common this particular issue is in their group I’ve done a lot of work
with law enforcement and emergency responders and they’re kind of their little group so
we talk about how common depression is among law enforcement and emergent emergency responders
specifically, because they face so much so many different stressors than you know Joe Schmo over
here so it D stigmatizes and normalizes a little bit now they still may not talk about it and
go well hey you know 37% of us have clinical depression no that’s probably not going to happen
but at least in the back of their mind, they can go you know what I’m looking around this room and
I can bet that at least one other person’s on antidepressants or something and feel a little
less unique and isolated in parent sessions you want to provide a rationale and overview of the
treatment model educates parents about the trauma and talks about the child’s trauma-related symptoms
so we’re going to go over what is hyper-vigilance what is the function it why people become
hypervigilant after trauma and what might it look like in a child because it presents very
differently for different children so we might want to give some ideas and say does this sound
like Johnny or does this sound like Johnny and help them understand why these behaviors may
be coming out we want to talk about how early treatment helps prevent long-term problems okay
maybe the trauma happened three years ago but still, it’s better than waiting ten more years and
you know Johnny’s still not having any Ellucian will want to talk about the importance of talking
directly about the trauma to help the children cope with their experiences and not hedging and
this will be on a case-by-case basis but the manual walks you through handling this discussion with
the parents about exactly how much detail do I go into if Johnny brings it up at home reassure
parents that children will first be taught skills to help them cope with their discomfort
and that talking about the trauma will be done slowly with a great deal of support so we’re not
just going to plop them down and go okay and tell me about the day that all this happened which
is what the child has experienced already if it was reported to law enforcement and/or the child
welfare they’ve probably had somebody sit down and say get right to the nitty-gritty at least
once or twice and it’s completely dehumanizing so we want to reassure parents that we’re not
going to do that to the child again will help the caregiver understand their role in the child’s
treatment since this modified since this model emphasizes working together as a team so I’m not
just going to be educating you it’s not going to be a parallel thing where I go in and I work with
Johnny and then I tell you what I did and then I work with Johnny I’m going to work with Johnny
and then we’re going to discuss what Johnny and I did in session and I’m going to get input from
you and we’re going to talk about how you feel about it and then I’m going to provide you with tools
so you can help Johnny outside of the session because you’re going to be with them for six-and-a-half
other days that I’m not and this can’t work if it’s just one hour once a week and we want to
elicit parent input questions and suggestions as much as possible because they’ve been living with
their kid for you know however many years so they probably have an idea about what works and what
doesn’t so we’ll start with both parents and children in their respective sessions helping
them understand what control breathing is and how it helps slow the heart rate and trigger the
wrist and digest sort of reaction in your body when your breathing slows your heart naturally
slows because the stress reaction tells your brain you’ve got to breathe fast and the heart
rates got to go fast well when you override that then you’re kind of overriding the whole system
and we’ll also talk about thought stopping and this is especially helpful if the trauma is recent
or and/or ever-present in the mind of the youth so they can say I am NOT going to talk about that right
now I’m not going to think about that right talk about distraction techniques go back to
your DBT stuff talks about improving the moment and accepts to help the child develop skills to
handle and work through when those thoughts pop up replace unthawed unwanted thoughts with
a pleasant one so talk about it in session when thoughts like that come up what would you
prefer to think about and then really get into the Nitty Gritty the five senses what do you see
smell hear taste you know help me get into that situation or that thought this teaches that
thoughts even unexpected and intrusive ones can be controlled so that gives them hope and again we’re
not exacerbating the thoughts right now we’re not bringing up their particular trauma and
having them get into detail we are just helping them deal with what’s happening normally on a
day-to-day basis so they feel like they have more control for the older kids you can have them
people log about when this technique is used what they were thinking about and how effective the
thought stopping was and then review it and help them tune it up if it’s not really effective and
give them praise for when they use it effectively relaxation training persons of Asian or Hispanic
origin tend to express stress in more somatic or physical terms so just be aware of that but that
doesn’t mean that Caucasians don’t relaxation training is good for anyone and the medical
school of South Carolina training recommended that relaxation is stress-free and
workbook by Davis Schulman and McKay so and it is still in publication when deciding how to
present relaxation techniques are creative have the child help you to integrate the elements
into the technique that makes it more relevant to them so, what are you thinking about when you
relax you know I know I like to go to the woods but maybe this kid likes to think about a video
game or play with their dog whatever it is but helps them make it relevant to them and then have
they identify other things they do to relax like drawing listening to music walking and making a
list of those things so they can refer to it when you’re teaching relaxation training especially if
you’re doing something like progressive muscular relaxation be sensitive to the child’s wishes if
they don’t wish to close their eyes or lie down which could trigger memories of the trauma we’re
not going there yet so if they feel vulnerable lying down or taking orders like that because
you can imagine how being told to lie down and close their eyes might be a trigger for certain
abuse survivors you know be cognizant of that and say you know get into a comfortable position
or how where would you like to sit while we talk about this like I said parents can often
benefit from the relaxation training as well so because they’re dealing with their issues
about the trauma but they’re also dealing with trying to figure out how to help Johnny and any
of them deal with any of Johnny’s misbehaviors or problematic behaviors then they move on to
feelings identification so it helps the therapist judge the child’s ability to articulate feelings
if you can tell me what makes you happy that’s great but if you can’t then you know we need to
work on figuring out what makes you happy you also want to help the child rate the intensity
of the emotion don’t let them stick with happy mad sad glad and afraid you know let’s talk about
different emotions and use the emotion chart with little faces on it or you can use the emotion
thermometer so is it a hot emotion or is it a cool emotion and helps the child
learn how to express feelings appropriately in different situations I mean sometimes they’re
going to be angry but it might not be appropriate to you know get up and stomp out of the room or
whatever however they communicate it so help them figure out how to articulate that so they can be
heard and supported some children have difficulty discussing or identifying their feelings so
you might try stepping back and discussing the feelings of other children or characters from
books or stories so you know think about Puff the Magic Dragon if they’ve read that you know
that dates me a little bit there but you know how did the little boy feel and talking about things
different characters and different stories where there are elements of anger and shame and loss and
all of that stuff helps children identify how they experience emotions if they seem detached
from the experience because sometimes they just they’ve shut it off it was just too overwhelming
so we want to talk about you know when you’re happy what does that feel like or when you’re
angry what happens what does your body feel like when you’re angry and they might be able
to tell you they hear their heartbeat in their ears or everything gets all fuzzy or whatever
but help them start tuning in to how they react and connecting that with an emotional word and then
after all, that’s done they can identify feelings they can identify feeling intensity now we want to
differentiate between thoughts and feelings many children describe thoughts when they’ve been
asked about a feeling so if you ask them how they feel they may say I want to run away so
you want to say okay well I hear that you want to run away so I’m wondering if you are bored and you
you’re bored and want to get away from it or if you’re scared can you tell me a little bit more
about what it means to you to want to run away during feelings identification the parent
sessions normalize what is going on with their child and help the parent understand that some
children may be seemingly in constant distress or detached from the trauma and that’s okay
we all react differently to traumas so again we’re going to share with the parents what we’re
Do let them know any specific difficulties if any juniors have encouraged the parent to praise
the child for appropriate management of difficult motions and I put in parenthesis successive
approximations because they’re not going to get it a hundred percent right every time so if they
try to effectively manage their emotions even a little bit let’s give them praise for that and
then help them figure out how to do it a little bit better the next time so instead of having a
complete meltdown maybe they got up and stomped out of the room well that’s an improvement so
then we want to talk about how to shape that behavior so it’s a more appropriate communication
if parents have difficulty identifying their own emotions provide them with examples so
continually ask them questions about how you feel when it’s a rainy day outside and how to do you
feel when somebody’s supposed to call you and they don’t how do you feel when and have about 15 or 20
examples and you can have them on a piece of paper and even give it to the parent to take home for
their homework if parents are overcome with their own emotions about the trauma validate
their feelings and explain how children need to see that their parents can handle talking
about the trauma so there the children need to see the strength and the parents which is what you’re
going to work on in parent sessions to make sure that the parents have the resolve and the skills
handle talking about this topic with junior TFC BT can be an effective intervention
for children or adolescents whose primary presenting issue is trauma-related emotional or
behavioral dysregulation TF CBT is not appropriate for clients who are actively suicidal and severely
depressed or currently abusing substances we want to make sure they’re clean
and sober as much as possible TF CBT starts with psychoeducation and then teaches stress
management and coping skills to aid in the management of distressing feelings psycho IDI
helps to clarify the inappropriate information children may have and start getting them a little
a bit more comfortable talking about the topic in general before we start going deeper and
feelings identification helps participants start effectively labeling and communicating their
feelings so they can receive the support and nurturance they need from their caregivers
and their support system if you enjoy this podcast please like and subscribe either in your
podcast player or on YouTube you can attend and participate in our live webinars with dr. Snipes
by subscribing to all CEUs comm slash counselor toolbox this episode has been brought to you in
part by all CEUs calm providing 24/7 multimedia continuing education and pre-certification
training to counselors therapists and nurses since 2006 use coupon code consular toolbox to
get a 20% discount on your order this month.