It is an honor and so much fun to be here and it’s been a lot of fun preparing this talk Each time I give this talk, things change and I learn more about the training program. You know I’ve been a psychiatrist for 25 years and when I first trained, I did an anxiety disorders fellowship and I started teaching about anxiety and anxiety disorders. And that was a hard topic to like get a big picture of and to do in an interdisciplinary way. And then I started working with addictions and teaching about that, and then gender and sexuality, and each one had its challenges in terms of how to teach residents and fellows about how to practice in some way. That was not just a cookbook, and you know cookie cutter about. This is how you treat this problem in this way, but I think that psychedelic, psychotherapy training has been the most challenging thing that I have ever undertaken and it continues to teach me a lot about doing therapy and being with patients and in teaching. So I’m going to try to cover several different topics. In my talk today, I want na ask the question: What is psychedelic psychotherapy And in particular, What is psychedelic psychotherapy that we do at NYU with our participants in the cancer anxiety study? I answered this question by looking at who was doing psychedelic psychotherapy today, who actively participates in offering and consuming psychedelic therapy, and also with some of the methods and techniques that are important, even if psychedelics are not involved. I’m gon na show a little bit about what it is that we do with participants that are in our study, and what kinds of experiences they undergo when they go through the work with us. I’m going to talk to you about how we train our therapists, what kinds of experiences we put them through, what kind of teaching we do, and how it is that we conceive of their going from one place to another. I want na ask the question: Why do we call it therapy a theme that you’re gon na hear me address throughout the talk today is why this is therapy and why we are not guides or monitors or sitters, but we are therapists who are Doing therapy with patients We call them participants or subjects, but for the clinical work that we are doing, it is therapists who are very well trained, who are sitting with human beings that are suffering, and we’re doing a short term therapy that has Psilocybin Sessions that are part of it – And I’m gon na close by asking What are the goals of our training program? What do we hope to accomplish in training people to work in the study? So what is Psychedelic Psychotherapy? It is a collection of psychotherapeutic processes that are facilitated by psychedelic agents, So the important part here is that psychedelic therapy has, as its basis a therapeutic process that already exists in the mind of the therapist and in many ways in the mind of the participant when They come in all of the experience all of the training that they’ve, had that patients or the participants experience in therapy. All of this comes to bear on what happens to people when they enter our research project in this way, it’s distinct from psychedelic agents as neuroscientific probes, into the function of the brain and the mind, and it’s also different in some important ways from psychedelic journeys that are undertaken for a recreational purpose or a spiritual purpose, or artistic creativity or individually. So this is a very specific therapy that’s done with people who are suffering from a certain condition. So what we do is not shamanic healing. It is not neo-shamanic healing. However, it does absorb many of the core teachings and the wisdom that come from those traditions. Psychedelic therapy is deeply embedded and inextricably embedded in the knowledge systems of the subject and the guide. Here we see Copernicus looking at the sky with a very primitive telescope and what Copernicus saw was the data that he gathered and how he interpreted. It was all very much based on what he knew about the heavens and what he thought was going on in the heavens. Now he may have seen things that surprised him that caused him to revise what he thought. But basically, what happened with that? Telescope was profoundly influenced by what he expected to see what he was surprised by and the basic knowledge base that was going on in his culture at that time. 300 years later, we have a much fancier instrument looking at the sky, but it’s more or less the same sky and more or less the same kind of instrument. But the way the data was gathered, the questions that were asked the way the data was manipulated and interpreted and the kinds of impressions that were drawn from it were very different. However, the same kind of instrument and the same kind of sky, So this shows how deeply it is in the mind of the observer and the looker and the person that’s participating in the experience that the catalyst or the technology which in our case is psychedelics. You know has to be understood, So I want to reintroduce the idea of psycholytic therapy. Psycholytic therapy is much referenced, but not that much talked about anymore. It’s a kind of therapy that was done in the Fifties and Sixties. It existed more in Europe than in America, although there was quite a bit of psycholytic therapy that happened here, in the modern psychedelic research Renaissance, there’s much more emphasis on psychedelic therapy, which is if you want na, be – and this is quite reductionist, Though, to say that psychedelic therapy has ego death brought about by the agent followed by a peak, spiritual or mystical experience, So this tends to be more unitary in the concept that is it’s more or less the same for everyone, and in fact, all of you Have probably seen the nine the list of nine criteria that define the mystical experience and in our study, we like to measure people to say how many of them they’ve accomplished. You know: do they get three or four or five, And if they get nine, then they’ve had a complete, mystical experience. So in this way, the idea is towards a kind of universal experience, and this is seen as having somewhat magical properties to heal. It brings about decreased death, anxiety, and transformation in character, which is seen, and it’s sort of a goal that people look for in research. However, it is a goal that is deeply bedded in contextualization. It’s more likely to happen with someone who’s prepared for it and who knows how to experience it. It’s not like it never happens in unprepared people, but in our study, people who have experienced meditators and have worked with ego death as it occurs in meditation retreats. That kind of person is more likely to experience ego death, followed by a spiritual or mystical experience, And this quasi-religious preparation is, you know, more likely to bring this about for this kind of individual, And in this case, the therapy supports the medicine experience. So the goal of the therapist in the context is to support this profound and shattering medical experience. Psycholytic therapy, on the other hand, is more biographical and more psychodynamic. It’s more individualized and has more to do with that individual’s, time on the earth and their experiences in childhood and adulthood, and it’s also deeply embedded in the relationship with the therapists who are in the room. In this way, the medicine supports the therapy experience and there’s a lot of writing that happened about psycholytic therapy that advanced whatever kind of therapy that patient and that therapist were doing in the Fifties and Sixties if they were Jungian therapists, if they were Freudian Therapists or Rogerian or relational therapists, the psychedelic experience used in a psycholytic manner advanced that particular kind of therapy. In our study, we measure and look for a mystical or spiritual experience, but many people have a combination of a psycholytic and a psychedelic experience, and some people have only a psycholytic experience, and this falls then, of course, to the therapists to interpret this and help. The patient, the ah participant works with it in a meaningful way To make this point one more time. Ana s, Nin said We don’t see things as they are. We see them as we are. So why is this point so important? Why do I hammer away at this point? Because when you teach a certain kind of therapy, you’re called upon to explain much of the basis of that therapy. How it works, why it works? What you’re doing, what distinguishes it from other kinds of therapy – and these are very difficult questions to answer about psychedelic therapy. For many reasons, One is that it’s not been done very much in the last forty years in an overground above-board way. And secondly, because there are so many different forms of psychedelic therapy. But when you want na teach something, especially in a rather traditional setting as we have at NYU, you have to have a matrix or a structure in which you’re setting out to teach a body of knowledge to therapists who don’t have it. So you have to decide What is the body of knowledge? What are we doing? Why are we doing it? Most people would agree that we are opening up something inside. So What are we opening up to with psychedelics? Why are we opening up to this? Why do we think it’s a good idea to unleash or open up these kinds of restrictions that happen in the brain, naturally, for a period of six or eight or ten, or twelve hours? Why was it closed in the first place? What are we looking for And are we instead opening up to something outside the self rather than inside the self? And these are all questions which it’s easy to ask. But when you teach it, it’s important to have some answers, and yet these are answers. We don’t have immediately at hand So an important question: How do we develop new narratives out of being involved in the study? That is How do the people who come to us for help come away feeling better feeling, like their life, is more meaningful, less afraid of death, and deeper engaged with the life that they have and able to know and experience that and speak of it? What can help these changes become long-lasting? All of these are questions that go into teaching psychedelic therapy and they’re questions that I wouldn’t say that I have all the answers to which makes it especially hard to teach And when you work at NYU or any academic setting, you have To make certain that what you’re doing fits into quite a traditional model of education, So part of the goal that we’re grappling with is how to develop a coherent model for teaching psychedelic-assisted therapy to conventionally trained therapists. All of the people that have been through our training program are trained and have extensive experience in working with patients, either as psychiatrists as psychologists, nurses, social workers, or family therapists. So they’re all fully trained therapists. And how do we teach this additional method? Or this additional kind of intervention, Or how do we teach therapists that know how to work with patients, then to use this new kind of experience using their unique skills and abilities and in some way trying to bring about a coherent treatment? Because if you’re saying This is psychedelic psychotherapy, you’re, defining it as something specific. You’re saying This is a certain kind of therapy. This is what it is, and this is what it is, ‘t and that kind of boundaries are problematic, if you think about things in a holistic way or a nondual way, that isn’t the way that psychiatry works. You know if you’re, defining a certain kind of therapy and you want na say have a fellowship in psychedelic psychotherapy. Then the chairman is gon na say Well. What is that, And how do you know it’s something, And how do you know when someone’s doing it, And how do you know when someone’s doing it well, And how do you know if somebody’s not doing it, but it Looks like they are, And these are all questions that you have to have at least practical answers to You also wan na answer, questions like Who can become a psychedelic therapist Who should become a psychedelic therapist And who shouldn’t. We tried to answer the question: How is our work different from the psychedelic therapy that’s done by underground workers, Of which hundreds? If not thousands, of sessions, are, ah, you know happening every year? And how do we integrate our training with the therapist’s existing approaches, And how do we bring our responsibilities, as you know, trained professional therapists to the psychedelic therapy setting? So this is the title of our study: Effects of Psilocybin, Assisted Psychotherapy on Anxiety and Psychosocial Distress. In Cancer Patients, This therapy occurs in a very specific context. It occurs in Manhattan at NYU. This is our research center in the upper right-hand, corner of the Bluestone Center for Clinical Research. People walk around with white coats on and stethoscopes around their necks, and so the people who come are, for the most part, very mainstream individuals who have cancer. Some of them quite advanced cancer. Some people are not too ill, but many people are quite ill and they’re involved with traditional cancer regimens with scans radiation chemotherapy, and these are the patients who come to us and enter our study by and large. These are the members of the NYU team, Steve Ross, who I think might be here in the room Steve Over there And Tony Bossis, who spoke on the first day of the conference, Gabby Agin Liebes, who might be here also over there And Carey Turnbull. Ah, director of development, Alexander Belser, who might be here, Alex No and Effie Nulman, another consultant and somebody who helps us with development – And this is an overview of our study for those of you who aren’t familiar with what it is we are doing. I thought I would show you what it is that the therapists do in our study and what it is that we’re preparing them to do. There are two dosing sessions: Dosing A and Dosing B. They’re, separated by seven weeks Before Dosing Session. There are three preparatory sessions. These are about two hours long. Then there’s Dosing Session, A which is either a placebo or an active drug. No one knows not the participant or the therapist or the PI or anybody. The only person who knows is the compounder who makes up the pill on a milligram per kilogram basis and puts it into a special envelope and then a special bottle and it’s all a very special audience. Laughter After Dosing Session A there’s a seven-week period and then there are integrative psychotherapy sessions Now if the person received a placebo or it appears to everyone that they got a placebo, then those next three sessions tend to be more continued preparation, because the experience With Psilocybin is the high point of the experience, so they either have in essence, six preparatory sessions and three integrative or three preparatory and six integrative sessions, And there’s a subtle. Well, you know not so subtle, dynamic differences that happen when a person is disappointed if they didn’t get an active drug first, but everyone knows that by the end of the study, they will have received a dosing session in both conditions. So, after the Dosing Session B, then there are about four weeks or five weeks during which there are three more integration sessions. So we have nine therapy sessions and two dosing sessions. Who are the psychedelic therapists of today To think about what we needed to learn, what we needed to do? I asked myself the question Who is doing work with psychedelics and who is doing work that feels related to psychedelic therapy, I came up with four categories: The Shaman, the Neo Shaman, the Meditation Adept and the Palliative Care Therapist, and the Psychodynamic Therapist of today, And I’m going to go through each one and talk a little bit about what we learned from them and what I think we needed to incorporate from these different disciplines. The shaman is the earliest and longest-lasting longest known psychotherapist in recorded history. A core of shamanism is communication with the spirit world. This occurs quite concretely. It’s, not a metaphor. It’s, not an aspect of the mind. It is a literal communication with spirits and the ability to work with unseen and mysterious forces and to intercede for the benefit of the sufferer is a core activity of the shaman. The shaman enters a trance state voluntarily, either with or without psychedelics, and experiences their soul or spirit, leaving the body or journeying or traveling on behalf of the individual, who is suffering The shaman interacts with spirits and will command intercede or commune with them in some way. To bring about a benefit for the individual who is in the ceremony or for the tribe or community as a whole, There’s quite a similarity between shamanic training and psychoanalytic training In both the individual by definition, suffers from some kind of malady. Some kind of unhappiness, frustration or fear, or anguish, some kind of suffering, which is both defined by and treated by a particular knowledge system. To become a psychoanalyst, you have to be, you know, upset neurotic troubled in some way by audience laughter seek treatment with an analyst, and undergo a genuinely therapeutic psychoanalytic process, And anybody who doesn’t do. That is probably not going to be very much good. As a psychoanalyst, enthusiasm for the method is a requirement for practicing it effectively also you learn a great deal about what it means to be a patient and what it means to be a therapist from working with your analyst. So the analyst, as well as the shaman, suffer from some kind of malady, and often both are, you know, marked at a very early age as headed towards a particular career. This is true for many therapists, And so this malady is cured or ameliorated in some way by shamanic practices or by psychoanalytic practice, and this is the embodiment of the wounded healer paradigm, in which the person who’s conducting the ceremony or conducting the analysis is Not expected to be perfect or flawless, but is expected to be someone who lives with a spirit wound and is working at healing it or has had it healed in some way and developed compassion and a unique ability to relate to other people. As a part of that process, Part of the culmination of a shamanic quest – and this is quite different from psychoanalytic training – is a confrontation with death. This confrontation with death, which often is accentuated in psychedelic experiences, is a catalyst for moving to a different stage of being without the encounter with death and the experience of dying either in a trans state. You know nonpsychedelic induced or with medicine the reaching out the hunger, the need, the expansion and extension of oneself to find a new way of relating to life to oneself doesn’t happen, And so it is this very terror and reaching through the sense Of groundlessness and shattering that transformation and rebirth can occur, And this is one of the things that is most important, I think for therapists to be able to work with participants in this study And to approximate this, we have a great deal of emphasis in The training process on confrontation with one’s, own mortality, fears about death and experiences of death and mortality in friends and family and patients The shamanic practitioner may take medicines and, as I’m sure everyone here knows, the practice may be that the shaman Takes the medicine and not the seeker or sufferer in their culture? That is not what happens in our study. It is the person with cancer anxiety who takes the medicine and the therapists in the room with him or with her are quite sober, although there is sometimes a kind of contagious experience of entering a trance with them, but we’re all sober pharmacologically speaking And in Shamanism psychedelic plants are considered gifts of the gods. They are mediators between the gods and humans and may carry special communicative potential, and it is also believed that it is the plant itself that is the god or the plant, contains the spirit power Mushrooms are found widely available in nature. If you know where to look – and you know when to look, They are not secreted away and they are not expensive. You just need to know what to do with them, where to find them, and how to use them In research. The molecules of Psilocybin are considered to be inert and to not have spirit within themselves, and yet they’re considered to be very dangerous and we had to install a very expensive and huge safe to protect a relatively small amount of Psilocybin. It’s weighed every day and there is some kind of danger that exists with the human beings around the Psilocybin because it needs this much protection. So, while these mushrooms are available growing in cow dung in certain places, when they arrive at First Avenue and 25th St, we need a big safe to keep everybody feeling. Okay, about it audience laughter. Now the shaman is a person who exists at the margins of society, but that doesn’t mean that he or she is a counter-cultural agent, because those who exist at the margins are very much a part of culture a part of society. The center can’t define itself if there isn’t a margin against which it can say. Well, we are not that, but we’re glad that person is here, because we can find what we don’t have in ourselves in them or we can hate them or we just need them in some way, But the shaman, perhaps a person marginalized in Society is a very well known and respected and valued person in society, so there are culturally bound narratives of illness and healing that the shaman knows and that the other members of the community know So even before a person goes to a shaman. What’s wrong? How it gets better, all these are cultural narratives that exist. You know as a part of the culture. There’s a highly ritualized training process, with a strong respect for tradition. So, although working with psychedelics is counter-cultural and edgy and kind of outlaws in the underground circles in the Western world, I think within indigenous cultures it’s not that way at all. There’s a training program. There’s an apprenticeship which I’ll talk about in a little bit and it also may be a part of the shaman’s job in a ceremony to reinforce pro-social values and social regulation and it’s. This function that’s thought to be significant in the ways that certain psychedelic-based religions facilitate recovery from alcoholism and other addictive disorders. Okay, so we’ve covered the indigenous shaman. Now I want to move on to the Neo shaman or Psychedelic Sitter. The training and practice for the Neo shaman are much less well defined. The practitioner may know of yoga may have a meditation practice, may do Chinese medicine or acupuncture, and uses intuition and many concepts from Transpersonal Psychology that are brought together as part of his or her method for doing psychedelic sitting or guiding The neo-shaman is generally naturally Emergent or self-selected A person says I would be willing to sit for you, and I believe that I have the credentials to do that or an individual may say I want you to do it And there’s little training or apprenticeship program that empowers the Sitter or the guide to know what they’re doing, except their own direct experience and reading and observing other people. The neo-shaman again has direct contact with the spirit world and enters into spirit reality through altered states and often in neo-shamanism. You see skepticism towards monotheistic religions, allopathic medicine, especially psychiatry, and overvaluation of the scientific method which is known as scientism, which is the irrational over belief in the scientific method and the belief that scientific knowledge is somehow harder or firmer or more powerful or more important or more Reliable than other kinds of truth, I’m not sure why this is capitalized. It shouldn’t be Neo. Shamanism is a descendant of the ideology of American Transcendentalism, which I’ll talk about in just a minute. Another distinction – and this is, of course, a generalization that shamanism there is generally a greater emphasis on searing pain, hardship, and terror than you see. You know by and large, in Neo shamanism, The Neo, shaman theory and methods are generally prohibited, prohibited discourse in medical circles. You know when you are talking to oncologists or nurse practitioners at the cancer center, and you start using the language of shamanism. You can see people start to roll their eyes and glaze over and stop listening to you, And so, since we’re trying to persuade them to refer patients to us and to take what we’re doing seriously. You know this whole discourse is prohibited, even though it may have a great deal of value in communicating with the subject in the study And so is the Neo Shaman. This discourse is not preferred in medical science, PET scans are preferred, And yet we have many people who are bridges, Stan Grof, famously bridged, psychiatry and Neo shamanism and no course or lecture on psychedelic therapy would be complete without giving credit to James Fadiman. Who’s written this extremely useful guide? The Psychedelic Explorer’s Guide and Neal Goldsmith his book, Psychedelic Healing, and numerous others, So the mindfulness adept? Ah, it was clear to us early on that many of the practices and teachings within meditation are important for us, as practitioners, and for the participants to know how to do. Meditation is a technique for developing the skill of mindfulness, focusing on self-regulation through careful attention. Focusing on immediate experience and developing curiosity, openness, and acceptance, One of the underlying themes that happen in existential anxiety is that there’s little context to speak about the terror rage and disappointment that occurs after the development of a cancer diagnosis or cancer treatment and the looking Away the encouragement to cope the encouragement to fight the encouragement to be positive. All of these draw attention away from the most difficult, painful searing, hard questions and processes that need to occur, and this capacity of curiosity, openness, and acceptance of what is that is central. Mindfulness is something that I thought was quite important: to bring to training. Mindfulness and meditation are established techniques for entering altered states of consciousness, with the idea that entering them can be inherently transformative and bring about an improvement in outlook mood, and connection to other people Nonjudgemental. Radical self-acceptance is also important in meditative practice, something which we bring to bear with each person as they prepare for their psychedelic experience And Psychodynamic Therapist. There are many many things that we could say about what a psychodynamic therapist knows how to do, but much of it is embedded in his or her training. One thing that I think cuts across all schools of psychotherapy is that we help the patient, develop, alternative meanings and narratives about life. We do that in different ways. We do that in different with different techniques, but we all hope to help someone have a better sense of what their life means and how they can speak to themselves and understand themselves in it, and in particular, here. Cancer, illness, and death Narrative therapy is a particular form of therapy, in which truth is not just something that is discovered objectively. It is something that is constructed in the development of a narrative between the speaker and the listener, and this is a theme that I think comes up again and again when trying to understand how to use psychedelics in working with cancer-related anxiety, Like the shaman and The neo shaman, the psychodynamic therapist, believes in unseen forces. We don’t call them spirits or ancestors that exist in the spirit world. We call them the Ego, the Superego, the Id internalized object, relations, and internalized schemas. Many many of these metaphors, I believe, are for the similar processes that occur, But again, the psychoanalyst and the psychodynamic therapist are trained to work with these forces and just like the shaman to intercede on the patient’s behalf. To try to make things better Within psychodynamic therapy, there is a deep commitment to a personal healing journey, and extensive work toward self-knowledge, and understanding of transference and countertransference. All of these are invaluable in working with patients in our study And there’s a long history that’s not hidden from the people who are here in this room, but certainly hidden within traditional psychiatric and psychoanalytic circles of using LSD and other psychedelics to Facilitate psychotherapy – and here are three books – This one in the right-hand corner. I’d never seen it before, and I was kind of intrigued to see it showing up in my Google Images search My Self and I, with its nice 60’s graphics. Now, psychodynamic therapy is very consistent with Western norms, medical ethical norms, and standards, so it fits in comfortably with what we’re trying to do. So before telling you about the structure of our program, I want na do one more theory-based excursion and talk about the set and setting. We often think about set and setting as the set being the participant’s intention and the setting where the therapy occurs in some ways, this is our setting Manhattan streets Bluestone. This is the couch that the sessions occur on, but I’d like to suggest that two other contexts are deeply influential in the work that we do, and these are existential psychotherapy and American Transcendentalism. In particular, we work with Victor Frankl’s, Logotherapy Logotherapy, I’m gon na try to reduce it to just a few soundbites as its core that life has meaning under all circumstances, even the most miserable ones, and this biography of Frankl, showing this concentration Camp march at the top, and then this very thoughtful image of him as a young man, I think, says volumes about how he came to develop this philosophy. He believes that our main motivation for living is our will to find meaning And that, when the search for meaning is blocked, there is psychological damage that occurs According to Frankl. We discover this meaning in three different ways.

Earlier today, Steve talked about meaning-making therapy, which is a kind of practical technique for bringing these philosophical ideas to bear in the clinical situation. So the meaning is discovered in three different ways: by creating a work or doing a deed. By experiencing something or encountering someone or by the attitude we take So by creating experiencing or taking an attitude, Frankl says that everything can be taken from Man, but one thing: the last of human freedoms: to choose one’s attitude in any given set of circumstances. This is his famous book Man,’s, Search for Meaning – and I want na point out now that Logotherapy is not a psychology of the mind. It’s not about the Id. The Ego. Psychology internalized objects, relations, developmental stages, and perinatal matrices, It’s not about. Oh, if you look, this is what we find like you, ‘re making a map. It is a therapy of action about the creation of meaning the intention choice and the creation of meaning And Irving. Yalom can’t be left out. American Transcendentalism is a philosophy and a form of literature that had its origins in the 19th century and some ways, lives on today. In the New Age movement, American Transcendentalism holds in the inherent goodness of both human beings and nature. Now this is quite different than Freudian psychology of the late 19th century and 20th century which said that the inherent nature of human beings is filled with steaming, cauldrons of Id and rage and libidinal energy that needs to be modified and modulated to fit with The demands of society, It’s quite different than American Transcendentalism, which says that the individual is pure and it is society that is corrupting American Transcendentalism is an inherently optimistic philosophy. There is a great deal of belief in the self and the self-identity, in creativity and infinite possibilities of the human soul. There’s a belief in spiritual progress and the interconnection of all beings, the immense grandeur of the soul, and that the interior is a source of goodness and wisdom. So I’d like to come back down to Earth now and tell you about the structure of the training program that we have, and this is the structure that we have used just in our last year of training, which is the third cycle of training that We’ve offered.

http://adgenie.gotop100.com/
http://topdogsrotator.com/r/leroymoco

https://flyby–buffy.blogspot.com/
This is Shira Schuster, who is soon to be a Ph.D. and has been my co-instructor in the course for this year and has been a tremendous help and creative force in putting the training program together. So there are three core aspects to the training program: a one-year mentorship with one of the three investigators in the study, Steve Ross, Tony Bossis, or myself, a didactic series and work with two study subjects. This is the schedule with which we began last year. It unfortunately, was blown to bits by Hurricane Sandy, but by about February we started to recover and get back on track to all the papers that we wanted to discuss, and I’m going to talk about the didactic first. I don’t have all of the didactic papers here summarized, but just a few of them. We start with this fabulous paper by Matt, Johnson and Bill Richards, and Roland Griffiths on the safety and basic medical knowledge of psychedelics. This paper covers what ten other papers would be needed to convey the information about who is eligible, and who shouldn’t be taken into treatment. What are the risks? What are the basic techniques? It’s a great paper and offered a tremendous amount of information in a quick, ah, not a quick, but in a concise way to people who were going through training. The next is a wonderful article by Alison Witte, no relation to Stephen who’s organizing our conference today. This is a paper that I found in a journal on holistic nursing. She worked with nurses, who had worked with people who were seriously ill in Eastern Kentucky in Appalachia, and she looked at who had spontaneous mystical experiences while they were in the hospital and what contexts led to their arising. What nurses did that facilitated people being able to have mystical experiences being able to talk about them and what kinds of things the nurses learned about? How to help the person utilize that mystical experience in their life afterward? She also, interestingly, talked about the impact on the nurse that was doing the listening and participating in the creation of this shared experience. So this is a really useful article, nothing to do with psychedelics, but is really about how you occasion a mystical experience. What do you do that enhances the likelihood of that happening? We did some historical papers looking at LSD, assisted psychotherapy, and the human encounter with death by Bill, Richards Stan Grof, and others, and Pahnke’s groundbreaking article on the transcendental mystical experience in the human encounter with death. We studied contemporary scholarship in psychedelic research, Roland Griffiths et al 39, s paper on Psilocybin, occasioning, and mystical experiences, and we took a crash course in Yalom and Frankl by studying this paper by Bill. Breitbart Psychotherapeutic Interventions at the End of Life, A Focus on Meaning and Spirituality. So here I think you’re hearing again the ongoing theme of the establishment of meaning as a core process, that we encourage our therapists to bring to people in the study, So that’s the didactic series. If you want a copy of it, I’d be happy to send it to you by email. The next part I want to describe is the mentorship program. The mentorship program is defined as just that, and not as supervision. We used the idea of supervision at first but decided that mentorship is better for several reasons. A mentor is more of a guide, a friend, and a supporter. There’s more equality in a mentoring relationship than in a supervisory relationship, And since all of the people that are trainees in our program are fully trained therapists, we felt that they were enhancing or developing or extending their skills rather than learning something from scratch. So we use the term mentorship. Also, there’s a certain amount of teaching that comes back the other way that can be quite profound, and I’ll tell you a little bit more about that later. The mentorship relationship is confidential. The mentor doesn’t say anything and holds the material found in the mentorship sessions, with equal confidentiality to what you would hear in therapy. The intention of the mentorship is an integration of all aspects of the experience. The trainee is encouraged to discover new aspects of himself or herself and others through the relationship. In other words, How does my existing identity as a therapist change grow to transform? What do I leave away? What do I do more of? How am I changed in this experience? In learning how to work with psychedelic therapies And a core part of the mentorship is dyad training. Now, when you work with two study subjects, which is a third part of the program, you work with your mentor for at least one of the sessions, So each therapy team each therapy dyad – has to do dyad training And the dyad training, which I’m, going To tell you about in a second is the central part of the mentorship relationship at the beginning, So you meet for these six two hour sessions, doing dyad training and by that time usually, you’ve gotten started working with your first patient, Your first participant So At that point, you’re doing clinical work. You’re talking about what’s going on. You’re talking about what’s happening in the reading, But the dyad training is a central way that the mentor and the trainee get to know each other. The dyad sessions occur six. There are six of them, They’re about one to one and a half hours, and only the therapists are present, so it’s a group of two and what happens in there also is confidential. Each session has a defined theme, even though you’re encouraged to do free-flowing discussion and talk about anything that arises that you think is going to be relevant to working together as a dyad team, And we used to have supervision after the third and sixth Sessions, but I think that’s pretty much fallen by the wayside, So the goal is the establishment of a close relationship. If you’re going to be a dyad team, you have to know one another as therapists. You have to understand how somebody thinks about life, death suffering, and when I first picked this picture, I thought that it was just kind of cutesy, but I realized that one of the times I’ve, given this talk before that there, something quite similar Between this tin can string telephone and that’s that you either are listening or speaking and to change, you have to change your position And the dyad sessions occur in the same way when you’re speaking, a person is expected to say what They have to say to describe their experience and the other person listens. It’s, not a therapy session. You’re not expected to ask questions to deepen the experience, But it’s a practice of a certain kind of meditation. Listening The first session early memories and contemporary experiences of death and losses, Family members, pets, friends, and patients that have died, Each person is invited to talk about their life from their earliest memories to the present time of what death and mourning has been like for them. This is also the time to talk about early memories of awareness of your mortality and thoughts and feelings about your death and the death of loved ones. The second dyad session is an invitation to talk about profound, mystical, or spiritual experiences, including experiences with entheogens. So confidentiality is also a part of the protection of this because speaking openly about entheogenic experiences or psychedelic use in a context like this brings about certain kinds of ethical and legal anxiety in people. So only with confidentiality, I think, are people free to speak openly about what they’ve done, what they’ve, not done, what it has meant to them, and the part of them that they’re going to bring to their dyad work, which is The work with the participant that relates to their own experience or lack of experience with entheogens. They can speak about their experience as a sitter and as a guide with shamans or guides or meditation teachers that they might have had. And this allows a basic kind of groundwork to be established between the dyad, as they’re, getting ready to sit with someone who’s going to enter into a state which is rather unpredictable in terms of what they’re going to be confronted with. Holding The third session involves looking at pain and suffering in family members, friends, and patients and experiences with cancer or other terminal conditions, including experiences in working with patients who are disfigured and whose bodies are failing, and the impact that this has ten minutes. Okay, so session. Four near-death experiences Session, five audience laughter beliefs regarding heaven and hell and religious history Session, six extreme states in psychotherapy, but actually by session six, everybody’s pretty much done and we’ve talked about everything there is to talk about So that’s, The one-year mentorship and I’m – going to skip over that and talk about the study and what happens during the sessions. So I presented this slide before, but I’m going to go over it again. You’ve got three prep sessions. A dosing session, three more sessions, a dosing session, and then three more So there are nine therapy sessions and two dosing sessions. The three preparatory sessions: this is the study room. This is what it looks like. This is a model pretending to be in session and the first prep session. So during the first prep session, it’s divided into two parts: there’s education to the participant regarding goals, the purpose of the study, time tables expectations, and education regarding the range of possible effects of the medication side, effects, rescue medications that we have On board what we’re going to do to try to help them through a difficult experience, and after that, then we do a history during which we take a psychosocial history, in particular a cancer narrative. We talk about family relationships, hobbies, work, political, social, and religious affiliations, the experience with psychedelics, meditation practice, and anything that you would want to do to get to know somebody and develop a trusting relationship with them. The second session is a life review. In this, we do a rather structured exercise, which I’ll show you an example of in just a minute, but you go over much of the same material you go over where you were born growing up where you went to school when your dad transferred to Another state: what happened when your grandmother died? You know if you had to go into the service like whatever these important turning points are in your life. We talk about them literally on a timeline and examine the meaning of those events in the individual’s life to see how their life has come to have meaning how events were made, the meaning of how catastrophe or disappointment or anger or exaltation moments were Given meaning and came to structure the way their life worked, In particular in the life review, we look at the cancer narrative, which has to do with how you reacted to the diagnosis, what the diagnosis meant and the relationship between cancer spirituality and how the individual found, Meaning So this is a life review exercise on the left hand, the side you can see birth about two-thirds of the way across you can see. Now this is a man in his late forties and on the very right-hand, side. He writes his death, So you can see between birth and now there’s. Many many events and I’ll give you a closeup in just a minute and about halfway through. You can see that he didn’t leave enough space, which is like the proportion wasn’t right. So he wrote a little. U going down to write in some more information, And this is a close-up of what he wrote At the bottom. He wrote his regrets loss of friends. He had to care for his mother when he had pneumonia. He was mean to Scott when he was a kid and did well in school and became a quarterback. All of these were things that he felt were important and just getting this information writing it here and taking this time was a profound experience for him each person that we work with says You know I’ve never done anything like this before and It’s quite illuminating to have these memories sought in this relatively structured way, And then the third is taking a spiritual history. To take the spiritual history, we use these two mnemonics, HOPE and FICA, and I’m gon na skip over this because I’m running out of time. But these you know information about these is easily available online, The spiritual history. What are your beliefs More about the spiritual history more about the spiritual history, The dosing sessions? Now I’m not going to say a great deal about the dosing sessions, because what we do is not vastly different than what is written about quite extensively. How do we handle people in various kinds of situations, what do we expect, what do we invite them to do, and how do we handle crises? This is quite extensively covered by many many people and what we do. Isn’t different from it. We have headphones with music. The therapists take a supportive role and respond actively if necessary. We have an opening ritual that focuses on internal direction and immersion in the inner experience. The therapists are invited to watch, listen and be attuned and very careful. Listening to the first post-journey, narrative, usually around two or three, the person sits up, takes off their headphones and eyeshades, and starts talking about what they’ve been through, and this first narration of the experience is quite important, and listening to it Carefully, I think, sets the ground for how you’re gon na work with it in subsequent sessions. Then you have a closing ritual So the integration sessions. These are the least well-defined part of the process, and they vary considerably from one dyad team to another, and while there is an effort in academic research to have uniformity and to have a manualized approach to things, I think that these integration sessions are a place Where it’s going to be quite a challenge to do this, because what the person brings, what happened to them in their session and who the therapists are and the bond that they’ve tied the bond that they’ve made. The tie that’s happened among the three of them is going to define what happens in the integration sessions So again making meaning of a psychedelic experience and incorporating that meaning into one 39. S perspective on yourself and in the world is an essential part of what we’re trying to do Now. This is Reverend Mike Young, and this is a slide that I didn’t know about this quote, and it was Cody Swift. That turned me on to this wonderful quote, and this is in some ways the idealized experience in which the ego, which is constructed by memory and determines what we think under Psilocybin. You transcend this ego. It’s not who I am, and the loss of self is not as distressing as it was before. So this is kind of the idealized experience and this is a picture actually of Marsh Chapel, where the Good Friday experiment happened, and people praying in that very same chapel. But not everybody has this full experience. Some people have a much more biographical experience and I don’t think I’ve read a description of what you need to do better than what came forward quite recently in this lovely small monograph by Torsten Passie. Describing what kinds of things can happen in a session – and I don’t think that much of what’s here is going to be new to anyone here, so I’m not going to go through this in the interest of time and again. Well, one point that I wanted to make about this is that Sometimes you hear you know when people are talking about Katherine MacLean’s report on openness that 14 months later, openness was found to be increased by a single psychopharmacological event, And when that phrase is Used it reduces the experience to the drug itself and I think that the mystical experience is sometimes seen as kind of like the magic that brings about some kind of transformation without being contextualized in a certain kind of therapeutic process. And I’d like to suggest that it really isn’t quite this way and that, even when a full mystical experience occurs, the way that it is held, the way that it is worked with the way that it is applied and connected to the individual.’s, life is very much a part of a therapeutic process that occurs So what have we learned from working with our trainees? This came out of a discussion that I had with Steve Ross and Tony Bossis a month ago, and I’ve got nine points that I want na make and that will bring me to the end of my talk. For today. There is a complex relationship between spiritual states, the cancer narrative, and experience with altered states. Now we hear these words – and these words are said a lot, but sitting with people and trying to figure out what their cancer narrative means to them, what their life meant and how life has meaning, how cancer affected the meaning in life and the relationship of Those two to this one psychedelic experience: these are like bridges that need to be made and they need to be made actively Just sitting back and saying. So what was it for? You are not going to bring about a very powerful connection unless it’s. Already happened So this complex relationship, I think, has much to be found and discovered about it, but it’s quite important. Secondly, that there’s a great variety in the way that spiritual distress and existential anxiety present themselves In general, the greater the mystical experience, the less active integration is needed. So this is what you know. Some of our mentors have felt that when there’s a more full mystical experience, the integration sort of happens on its own or kind of happens. Naturally, When it’s less and there’s more of a biographical or psychodynamic, then more dynamic work is needed. Number four involvement, as a therapist in a study, brings about deep personal changes in the relationship to cancer, death, and therapeutic stance. For me, this had to do with facing patients who were dying and talking about dying. Looking at my feelings about death, illness, pain, cancer pain, and my mother,’s, death from cancer. All of this got activated in me and I realized how much I had been living. You know once or twice removed from these very deep existential issues, because when you work with addictions, you’re almost always working with somebody who’s going to have a new birth and a new life in sobriety, and there’s much of a hopeful Perspective so this reduction in lifespan and the threat of dying from cancer brought about a change for me. On the other hand, I work in my therapy dyad with somebody who’s been working in cancer care for 15 years, and her attunement to defenses denial around cancer, anxiety, diagnosis, anxiety. The way that somebody hears or doesn’t hear information that they’ve got is very, very refined for her imagining this new technique. This new way of helping a certain kind of suffering that she was so familiar with was quite different for her. It is like What is a psychedelic experience for this particular patient, going to do for this very familiar form of cancer care that she’s done? Number five – and you know this – is like beating a dead horse. The centrality of the construction of meaning healing existential anxiety due to cancer. Core processes that were necessary for the therapist are the cultivation of authentic presence, meditative attention, and balance between overactivity and overinvolvement, usually caused by anxiety in the therapist or detachment, which can be caused by an overvaluation of a certain kind of calm or a certain kind of meditative Observation when a more engaged or forward-leaning approach might be helpful and the skills helpful in bringing about a mystical experience Each therapist’s. The trajectory is embedded in his or her past and path and there’s a great value. When you’re doing short-term therapy like this, to know how to work with patients to know about transference and countertransference and skill about what to open up what to leave closed, how to work with things that emerge how to work with crises that arrive, how To handle the subtle and important things, that you might not recognize, or you might not notice, if you weren’t well trained there’s a great deal of value in being a well trained, therapist And number nine. The unquestioned value of personal experience with entheogens in working with integrative sessions, especially in working with difficult passages during dosing sessions. So I’m going, to sum up with two slides, So I want to talk about the goals of the training program. There are two sets of goals: One is the goals for the therapist, so you know the goals that go in, and the other is goals that go out. The goal of the training program for therapists is to develop the capacity to support spiritual and mystical experiences in the subject and to relate these to illness and mortality and existential anxiety So to conduct short-term therapy, work that integrates spiritual experiences and facilitates psycholytic work. So these are a lot of words to encapsulate what I think is the core task of what we’re trying to do, and that is to be both psychedelic therapists and psycholytic therapists and short-term dynamic, psychotherapists. The therapist’s goal is to become safe, skilled, and knowledgeable in all aspects of the process, meaning patient selection, patient preparation handling the session, and whatever occurs in the psychedelic session and the integration that happens afterward, whether that’s three or six sessions or For several years, which can occur, you know one of the people who were in our research study stayed in treatment with her dyad for several years, because it was just clinically the best thing to do So being able to know when to do what is a very important part of adding this kind of technique to your work And, lastly, to support each therapist’s, talent, maturity and individuality and to practice therapy that is creative, adventuresome and unknowing. And by that I mean where the therapist is comfortable with not knowing what’s going to happen, not knowing what should happen but having an open mind and an open heart to be ready to respond to what does happen And the external or the far-reaching Goals for the training program: these are out for the community First to define a training process and evaluate its effectiveness in an ongoing way. So we had to develop a training program before or you know, without any training ourselves and without actually having done very much psychedelic psychotherapy in this particular context. So we sort of hit the ground running and now by the third round of training, and we’ve done twenty-five subjects in the study. I’m starting to have some preliminary ideas about what’s effective in training. What’s important? What’s not so important, So creating a training process was an essential part of what I was trying to do, and to do this, I just started with one that I thought up and did and said: Okay, how is this working? What’s important and what’s not The next is to provide education and normalization of psychedelic discourse within the highly traditional medical setting. So in this study, the information goes out to departments of psychiatry departments of oncology. We have a journal club, the PGY 4 39. S sometimes comes to our lectures and the fellows in addiction, psychiatry, and in other fellowships, are invited to attend. So there’s a place where psychedelic medicine is being taught and talked about, and when we go to the cancer center. We talk about this. So, even though only twenty-five people have enrolled in our study and received dosing, hundreds and hundreds, if not thousands, of people in the NYU area have heard about the study and are seeing psychedelic medicines being taken seriously and being studied in a rigorously academic way. Thereby creating a conversation for reintroducing these agents into our discourse. The third is to prepare the needs for a Phase III study in which we would be doing two or three or even four hundred subjects in the study. So we’d need a lot of therapists for that and third to establish at least one model for a post-rescheduling world. In other words, if we were going to have Psilocybin offered as a form of therapy and therapists were going to offer it, how will they be trained? What will that therapy look like? How will we know when someone’s a good psychedelic therapist and somebody’s not pulling their weight or not doing a good job, And with that we’ll bring it to the end. Thank you very much.
As found on YouTubeHUMAN SYNTHESYS STUDIO 👀🗯 Attention: Have Real Human Spokespeople In Your Videos Saying Exactly What You Want In MINUTES! REAL Humans, REAL Voices, With A NEW Technology That Gives STUNNING Results Choose Your
Human + Voice Type What You Want Them To Say Render your “Humatar” What You Are About To See Is Unbelievable…
 Which means the brain’s
ability to adjust and adapt as well as learning and memory so these are good receptors I like
them glutamate binds with these receptors and high levels of glutamate are secreted during high
levels of stress glutamate remember is what GABA is made from but high levels of glutamate
it’s an excitatory neural net in the brain and overexposure of neurons to this glutamate can be
excited toxic and may contribute to the loss of neurons in the hippocampus of patients with PTSD
so we’re actually seeing brain volume decrease as a result of exposure to certain chemicals elevated
gluten core glucocorticoid and yeah glucocorticoids increases the sensitivity of these receptors so
you’ve got a bunch of glutamate being dumped and you’ve got a bunch of glucocorticoid you’ve got
cortisol in there making these receptors more sensitive so it’s got they’re more sensitive and
they’ve got more coming in which makes it a whole lot easier to become toxic and start causing
neuronal degradation what does that mean why do we care it may take clients with PTSD more time to
master new skills because of emotional reactivity but also because some of their synaptic plasticity
may be damaged so it may take them a little bit longer to actually acquire and integrate these
new skills it’s not saying they’re stupid they can remember it just fine however when they’re
an emotionally charged state and helping their brain learn that okay this isn’t a threat that’s one
of those sort of subconscious things that has to happen that can take longer if the brain becomes
excited toxic during stress inhibited learning and memory then it becomes excited toxic during
stress which inhibits learning and memory so it’s under stress things are excited toxic neurons
are starting to disappear so I’m wondering and I’m just hypothesizing here I don’t know the
answers obviously or I wouldn’t be practicing it but what happens during the exposure therapies
because that’s exactly what we’re doing is we are flooding the brain with all of these chemicals
and creating basically an excitotoxin now they found some evidence that exposure therapies can
be helpful according to the DOJ website but or not the DOJ I can’t even think of it right
now the VA website but you know I’m wondering long-term what the impact is endogenous opioids
natural painkillers act upon the same receptors activated by exogenous opioids like morphine and
heroin exerts an inhibitory influence on the HPA axis well we know that people take opiates
and it has depressant effects on them it slows them down and calms them down alterations in our
natural opioids may be involved in certain PTSD symptoms such as numbing stress-induced analgesia
and dissociation again think of any clients you’ve had who have been abused or even taken and not like
the side effects of opiates are what opiates do to some people make them feel more relaxed stress
induced and analgesia they don’t have as much physical pain sometimes they just it’s there
I don’t care pill another interesting factor is now truck zone which is used to oppose opiate
appears to be effective in treating symptoms of dissociation flashbacks in traumatized persons so
basically, they’re saying if we undo the endogenous opioids we can treat these symptoms it highlights
the risk of opiate abuse for persons with PTSD though because if endogenous opioids produce
some of these numbing symptoms and dissociative symptoms so they can get away from the pain and
the flashbacks then if they add to that you know oral opioids it could prove to be a very tempting
cocktail we do want to as clinicians figure out how we can assist them with their physical and
emotional distress tolerance so they don’t feel the need to numb and escape and you know I
can’t imagine what some people have seen have gone through and I’m not trying to take that away
from them, I’m trying to help them figure out how they can stay present and learn to integrate it
changes question marks in brain structure and one of the questions that’s come up in the research is
because there aren’t any longitudinal studies that looked at it was the hippocampal volume as low to
begin with which created a predisposition for PTSD or did PTSD create the smaller hippocampal volume
interesting hippocampus is implicated in the control of stress responses memory and contextual
aspects of fear conditioning so it helps you to find these triggers in the environment that
help you become aware with your senses about when there might be a trauma prolonged exposure
to stress and high levels of glucocorticoids damage the hippocampus we’ve talked about that
hippocampal volume reduction in PTSD may reflect the accumulated toxic effects of repeated exposure
to increased cortisol levels what I called earlier the flatter the Furious having you know your body
holding on to cortisol for this extreme stress and then when it perceives stress it’s either
nothing or it’s extreme there are no kind sort of mild stressors out there that decrease hippocampal
volumes might also be a pre-existing vulnerability factor for developing PTSD the amygdala yet
another brain structure is the Olympic structure involved in the emotional process and it’s
critical for the acquisition of fear responses functional imaging of studies has revealed hyper
responsiveness and PTSD during the presentation of stressful script cues or trauma reminders but
also patients show increased amygdala responses to general emotional stimuli that are not trauma
associated such as emotional faces so they show an increased responsivity to things they see on the
TV that aren’t trauma-related to people crying to people showing anger’s going to have a
stronger emotional amygdala response than people without PTSD so clients with PTSD may be more
emotionally responsive across the board leading to more emotional dysregulation again an area that
we can help provide them with tools for early adverse experiences including prenatal stress and stress
throughout childhood has profound and long-lasting effects on the development of neurobiological
symptoms the brain is developing and if is exposed to a lot of stress and some of these excited toxic
situations how does that differ in the amount of damage caused versus a brain that’s already kind
of pretty much-formed programming may change for subsequent stress reactivity and vulnerability
to develop PTSD so if these happen during childhood or at any time the brain can
basically reprogram and go that it’s a really dangerous place out there so I need to hold
on to cortisol and I need to hold on to these stress hormones because every time I turn around
it seems like there’s a threat so I am going to be hyper-vigilant and respond in an exaggerated way
to protect you from the outside world adult women with childhood trauma histories have been shown
to exhibit sensitization of both neuroendocrine and Audino stress responses so basically they’re
showing hypo cortisol ISM a variety of changes take place in the brains and nervous systems of
people with PTSD and we talked about a lot of those the key take-home point is stress can
actually get toxic in the brain and cause physical changes not just thought changes in the brain
preexisting issues causing hypo cortisol ism where the brain has already downregulated whether it’s
due to chronic illness or chronic psychological stress increases the likelihood of the development
of PTSD this points to the importance of prevention and early intervention of adverse
childhood experiences we really need to get in there and help these people develop distress
tolerance skills understanding of vulnerabilities so they’re not going from flat to furious all
the time and so that they can understand why their body kind of responds and why they respond
differently than others and you know as we talk about this and of course I’m regularly bringing up
DBT buzzwords if you will think about your clients if you’ve worked with any who’ve had borderline
personality disorder what kind of history do they have did they have just a great childhood no we
know that people with BPD generally had pretty chaotic childhoods so this research is also
kind of underscoring why they may react and act the way they do that flat to furious people with
hypo cortical ism may or may not have PTSD so we don’t want to say well you’re fine if you don’t
have PTSD symptoms we do know that every trauma potentially can cause the body to down-regulate
and I kind of look at it as conserving a little bit more of the energy that it needs each time so
instead of conserving 60% now it’s conserving 65 and 66 each time it encounters a stressor in order
to prepare for potential ongoing threats in the environment hypercortisolism sets the stage for
the flattened the furious leading to toxic levels of glutamate upon exposure to stressors which
can cause the theorized reduction in hippocampal volume and persistent negative brain changes now I
always say the brain can you know rebalance itself and all well that’s part of the plasticity that is
the really cool thing about our brain however as far as regenerating those neurons I haven’t found
any evidence in the research that we found a way to help people regenerate once we’ve already those
neurons are gone they’ve been killed off the brain has to find a workaround so it does take time
but I do believe people can minimize some of the impact of the trauma they may have experienced
people with PTSD are more reactive to emotional stimuli even stimuli unrelated to trauma again
think about some of your clients especially if you work in a residential situation where you’re
around on 24/7, you know for 30 or 60 days, and you may see some clients that seem to get upset
over everything and you’re like ah such a drama queen or such a drama king and to yourself not
to anybody else but when you think about it from this perspective it gives you a different
perspective and you might say oh maybe their body responds differently they’ve got more emotional
dysregulation because of prior trauma they’re not trying to overreact this is their body’s response
because it’s perceived threat so many times it gives me a different approach to working
with that client hypercortisolism results when the brain perceives that continued effort is futile
feelings of fatigue set in akin to reduced stress tolerance so think about you know when you’ve had
a really long stressful period you know weeks or months maybe you’re dealing with an ailing family
member or something it’s just a lot of stress and you start getting really tired and when you’re
really tired and you’re worn down and somebody gives you one more thing it’s that one more thing
normally wouldn’t bother you but right now you just can’t take it so we can see how there’s a
reduced stress tolerance when somebody’s already at this stage reducing fatigue in our clients can
be accomplished in part with psychological factors including motivation or knowledge of other people
who are dealing with similar things support groups feedback about their and making sure they have
frequent successes not once a week but I want to have them keep a journal every day of something
good that happened or something positive that may indicate they’re moving forward in their
treatment goals and knowledge of an endpoint.
Which means the brain’s
ability to adjust and adapt as well as learning and memory so these are good receptors I like
them glutamate binds with these receptors and high levels of glutamate are secreted during high
levels of stress glutamate remember is what GABA is made from but high levels of glutamate
it’s an excitatory neural net in the brain and overexposure of neurons to this glutamate can be
excited toxic and may contribute to the loss of neurons in the hippocampus of patients with PTSD
so we’re actually seeing brain volume decrease as a result of exposure to certain chemicals elevated
gluten core glucocorticoid and yeah glucocorticoids increases the sensitivity of these receptors so
you’ve got a bunch of glutamate being dumped and you’ve got a bunch of glucocorticoid you’ve got
cortisol in there making these receptors more sensitive so it’s got they’re more sensitive and
they’ve got more coming in which makes it a whole lot easier to become toxic and start causing
neuronal degradation what does that mean why do we care it may take clients with PTSD more time to
master new skills because of emotional reactivity but also because some of their synaptic plasticity
may be damaged so it may take them a little bit longer to actually acquire and integrate these
new skills it’s not saying they’re stupid they can remember it just fine however when they’re
an emotionally charged state and helping their brain learn that okay this isn’t a threat that’s one
of those sort of subconscious things that has to happen that can take longer if the brain becomes
excited toxic during stress inhibited learning and memory then it becomes excited toxic during
stress which inhibits learning and memory so it’s under stress things are excited toxic neurons
are starting to disappear so I’m wondering and I’m just hypothesizing here I don’t know the
answers obviously or I wouldn’t be practicing it but what happens during the exposure therapies
because that’s exactly what we’re doing is we are flooding the brain with all of these chemicals
and creating basically an excitotoxin now they found some evidence that exposure therapies can
be helpful according to the DOJ website but or not the DOJ I can’t even think of it right
now the VA website but you know I’m wondering long-term what the impact is endogenous opioids
natural painkillers act upon the same receptors activated by exogenous opioids like morphine and
heroin exerts an inhibitory influence on the HPA axis well we know that people take opiates
and it has depressant effects on them it slows them down and calms them down alterations in our
natural opioids may be involved in certain PTSD symptoms such as numbing stress-induced analgesia
and dissociation again think of any clients you’ve had who have been abused or even taken and not like
the side effects of opiates are what opiates do to some people make them feel more relaxed stress
induced and analgesia they don’t have as much physical pain sometimes they just it’s there
I don’t care pill another interesting factor is now truck zone which is used to oppose opiate
appears to be effective in treating symptoms of dissociation flashbacks in traumatized persons so
basically, they’re saying if we undo the endogenous opioids we can treat these symptoms it highlights
the risk of opiate abuse for persons with PTSD though because if endogenous opioids produce
some of these numbing symptoms and dissociative symptoms so they can get away from the pain and
the flashbacks then if they add to that you know oral opioids it could prove to be a very tempting
cocktail we do want to as clinicians figure out how we can assist them with their physical and
emotional distress tolerance so they don’t feel the need to numb and escape and you know I
can’t imagine what some people have seen have gone through and I’m not trying to take that away
from them, I’m trying to help them figure out how they can stay present and learn to integrate it
changes question marks in brain structure and one of the questions that’s come up in the research is
because there aren’t any longitudinal studies that looked at it was the hippocampal volume as low to
begin with which created a predisposition for PTSD or did PTSD create the smaller hippocampal volume
interesting hippocampus is implicated in the control of stress responses memory and contextual
aspects of fear conditioning so it helps you to find these triggers in the environment that
help you become aware with your senses about when there might be a trauma prolonged exposure
to stress and high levels of glucocorticoids damage the hippocampus we’ve talked about that
hippocampal volume reduction in PTSD may reflect the accumulated toxic effects of repeated exposure
to increased cortisol levels what I called earlier the flatter the Furious having you know your body
holding on to cortisol for this extreme stress and then when it perceives stress it’s either
nothing or it’s extreme there are no kind sort of mild stressors out there that decrease hippocampal
volumes might also be a pre-existing vulnerability factor for developing PTSD the amygdala yet
another brain structure is the Olympic structure involved in the emotional process and it’s
critical for the acquisition of fear responses functional imaging of studies has revealed hyper
responsiveness and PTSD during the presentation of stressful script cues or trauma reminders but
also patients show increased amygdala responses to general emotional stimuli that are not trauma
associated such as emotional faces so they show an increased responsivity to things they see on the
TV that aren’t trauma-related to people crying to people showing anger’s going to have a
stronger emotional amygdala response than people without PTSD so clients with PTSD may be more
emotionally responsive across the board leading to more emotional dysregulation again an area that
we can help provide them with tools for early adverse experiences including prenatal stress and stress
throughout childhood has profound and long-lasting effects on the development of neurobiological
symptoms the brain is developing and if is exposed to a lot of stress and some of these excited toxic
situations how does that differ in the amount of damage caused versus a brain that’s already kind
of pretty much-formed programming may change for subsequent stress reactivity and vulnerability
to develop PTSD so if these happen during childhood or at any time the brain can
basically reprogram and go that it’s a really dangerous place out there so I need to hold
on to cortisol and I need to hold on to these stress hormones because every time I turn around
it seems like there’s a threat so I am going to be hyper-vigilant and respond in an exaggerated way
to protect you from the outside world adult women with childhood trauma histories have been shown
to exhibit sensitization of both neuroendocrine and Audino stress responses so basically they’re
showing hypo cortisol ISM a variety of changes take place in the brains and nervous systems of
people with PTSD and we talked about a lot of those the key take-home point is stress can
actually get toxic in the brain and cause physical changes not just thought changes in the brain
preexisting issues causing hypo cortisol ism where the brain has already downregulated whether it’s
due to chronic illness or chronic psychological stress increases the likelihood of the development
of PTSD this points to the importance of prevention and early intervention of adverse
childhood experiences we really need to get in there and help these people develop distress
tolerance skills understanding of vulnerabilities so they’re not going from flat to furious all
the time and so that they can understand why their body kind of responds and why they respond
differently than others and you know as we talk about this and of course I’m regularly bringing up
DBT buzzwords if you will think about your clients if you’ve worked with any who’ve had borderline
personality disorder what kind of history do they have did they have just a great childhood no we
know that people with BPD generally had pretty chaotic childhoods so this research is also
kind of underscoring why they may react and act the way they do that flat to furious people with
hypo cortical ism may or may not have PTSD so we don’t want to say well you’re fine if you don’t
have PTSD symptoms we do know that every trauma potentially can cause the body to down-regulate
and I kind of look at it as conserving a little bit more of the energy that it needs each time so
instead of conserving 60% now it’s conserving 65 and 66 each time it encounters a stressor in order
to prepare for potential ongoing threats in the environment hypercortisolism sets the stage for
the flattened the furious leading to toxic levels of glutamate upon exposure to stressors which
can cause the theorized reduction in hippocampal volume and persistent negative brain changes now I
always say the brain can you know rebalance itself and all well that’s part of the plasticity that is
the really cool thing about our brain however as far as regenerating those neurons I haven’t found
any evidence in the research that we found a way to help people regenerate once we’ve already those
neurons are gone they’ve been killed off the brain has to find a workaround so it does take time
but I do believe people can minimize some of the impact of the trauma they may have experienced
people with PTSD are more reactive to emotional stimuli even stimuli unrelated to trauma again
think about some of your clients especially if you work in a residential situation where you’re
around on 24/7, you know for 30 or 60 days, and you may see some clients that seem to get upset
over everything and you’re like ah such a drama queen or such a drama king and to yourself not
to anybody else but when you think about it from this perspective it gives you a different
perspective and you might say oh maybe their body responds differently they’ve got more emotional
dysregulation because of prior trauma they’re not trying to overreact this is their body’s response
because it’s perceived threat so many times it gives me a different approach to working
with that client hypercortisolism results when the brain perceives that continued effort is futile
feelings of fatigue set in akin to reduced stress tolerance so think about you know when you’ve had
a really long stressful period you know weeks or months maybe you’re dealing with an ailing family
member or something it’s just a lot of stress and you start getting really tired and when you’re
really tired and you’re worn down and somebody gives you one more thing it’s that one more thing
normally wouldn’t bother you but right now you just can’t take it so we can see how there’s a
reduced stress tolerance when somebody’s already at this stage reducing fatigue in our clients can
be accomplished in part with psychological factors including motivation or knowledge of other people
who are dealing with similar things support groups feedback about their and making sure they have
frequent successes not once a week but I want to have them keep a journal every day of something
good that happened or something positive that may indicate they’re moving forward in their
treatment goals and knowledge of an endpoint. Where are we going with this when is the treatment
going to end I don’t want most clients don’t want to be with us forever no matter how lovable
we are do you want to feel better and be done with us so having to help them see that there
is an endpoint we’re going to accomplish this goal this month and then we can reassess 46% of
people in the US are exposed to adverse childhood experiences so like I said this is a huge area
for early intervention where we can prevent people from developing PTSD later in life how awesome
would that be instruction and skills to handle emotional dysregulation including mindfulness
vulnerability prevention and awareness emotion regulation distress tolerance and problem-solving
could be wonderful additions to health curriculums anything any skills groups you do with children
or adolescents or even adults I mean just because they’re adults doesn’t mean that they’re safe
from PTSD or that they’ve crossed any threshold where they’re too old to learn we’re never too
old to learn of those exposed to trauma education about and normalization of their heightened
emotional reactivity and susceptibility to PTSD in the future may be helpful in increasing their
motivation for their current treatment protocol whatever it is but it also just normalizes things
so they don’t feel like they’re overreacting or they don’t feel guilty for being so tired
or whatever they’re experiencing right now are there any questions I know I went through
a lot of really complicated stuff but I thought it was really interesting not only the way
our brain reacts in order to protect us but how cross-cutting a lot of this stuff
was it not just PTSD we’re talking about necessarily but a lot of this information
applies to our clients with chronic fatigue burnout and chronic stress and we can
see that those people also are at risk at higher risk of PTSD should they be exposed
to trauma and none of us is immune I mean there are tornadoes there are hurricanes
there are you know things that happen that really stink so the more we can help clients
be aware of things develop skills and tools to prevent as much harm as possible I
think the more effective we are as clinicians depending on the client and I can do some
more research on the VA website because they’re really into medications for PTSD I
know ketamine which is a horse tranquilizer has been shown to be effective in people
with PTSD and there have been some others that have kind of given me pause ketamine
is a hypnotic you know most of the drugs they’re trying out right now are really in my
opinion they’re powerful drugs but a lot of them all of them that I know of have
pretty high addictive potentials too so they make me nervous but you know when you’re
weighing the when you’re going from a harm reduction model that’s not necessarily not
necessarily such the be-all-end-all I guess that’s interesting that you use ketamine in the ER it’s definitely powerful effective stuff and like I said earlier some of the
stuff that some of my clients and some people have seen done experienced I couldn’t even
imagine and you know sometimes for them to actually survive we may need to look at some
of these more intense more powerful drugs PTSD and veteran trauma is not are not my focus
right now and yes marijuana is being experimented with or looked at used whatever however you want
to look at it for PTSD treatment with veterans there’s pretty much not a drug out there they
haven’t tried to throw at it to see well what will this do I believe they were even using
LSD experimentally for a little while too you the VA I mean if you’re interested in this
topic let me see if I could pull that down into here, we go to the National Center
for PTSD US Department of Veterans Affairs has a lot of information if you go for
professionals, it has a ton more information if you can get on get some of your SI CEUs on
demand they do have some free CEUs for PTSD here I’ve never taken any of them but what
I’ve looked at when I’ve looked at like the PowerPoints the presentations and stuff I’m
sure they’re good so if you’re you do focus a lot on PTSD and you can get on-demand CEUs
then this might be a place to get some good free ones aside from DBT are there any other
evidence-based practices for therapy that you’ve seen work best in combination with the
medications cognitive processing therapy when you’re working specifically with veterans
and there is a free course on that too and this one I have gone through
and it’s really awesome CPT dot must seed and here I’ll just put it
into that education and this is a free course oops and here’s the other one ah golly everyone and
embryo does have a lot of research effectiveness with people with PTSD too so yes I would
definitely encourage people to explore all options alrighty everybody I really
appreciate you coming today and sticking with me through this topic and I will see
you on Thursday if you have any questions please feel free to email me or you can
always also send it to support that all CEUs com either way I get it and otherwise I
will see you on Tuesday thanks a bunch if you enjoy this podcast please like and
subscribe either in your podcast player or on YouTube you can attend and participate
in our live webinars with Doctor Snipes by subscribing at all CEUs comm slash
counselor toolbox this episode has been brought to you in part by all CEUs
com providing 24/7 multimedia continuing education and pre-certification training to
counselors therapists and nurses since 2006 used coupon code consular toolbox to get
a 20% discount on your order this monthAs found on YouTube15 Modules Of Intimate Video Training With Dr. Joe Vitale – You’re getting simple and proven steps to unlock the Awakened Millionaire Mindset: giving you a path to MORE money, …
Where are we going with this when is the treatment
going to end I don’t want most clients don’t want to be with us forever no matter how lovable
we are do you want to feel better and be done with us so having to help them see that there
is an endpoint we’re going to accomplish this goal this month and then we can reassess 46% of
people in the US are exposed to adverse childhood experiences so like I said this is a huge area
for early intervention where we can prevent people from developing PTSD later in life how awesome
would that be instruction and skills to handle emotional dysregulation including mindfulness
vulnerability prevention and awareness emotion regulation distress tolerance and problem-solving
could be wonderful additions to health curriculums anything any skills groups you do with children
or adolescents or even adults I mean just because they’re adults doesn’t mean that they’re safe
from PTSD or that they’ve crossed any threshold where they’re too old to learn we’re never too
old to learn of those exposed to trauma education about and normalization of their heightened
emotional reactivity and susceptibility to PTSD in the future may be helpful in increasing their
motivation for their current treatment protocol whatever it is but it also just normalizes things
so they don’t feel like they’re overreacting or they don’t feel guilty for being so tired
or whatever they’re experiencing right now are there any questions I know I went through
a lot of really complicated stuff but I thought it was really interesting not only the way
our brain reacts in order to protect us but how cross-cutting a lot of this stuff
was it not just PTSD we’re talking about necessarily but a lot of this information
applies to our clients with chronic fatigue burnout and chronic stress and we can
see that those people also are at risk at higher risk of PTSD should they be exposed
to trauma and none of us is immune I mean there are tornadoes there are hurricanes
there are you know things that happen that really stink so the more we can help clients
be aware of things develop skills and tools to prevent as much harm as possible I
think the more effective we are as clinicians depending on the client and I can do some
more research on the VA website because they’re really into medications for PTSD I
know ketamine which is a horse tranquilizer has been shown to be effective in people
with PTSD and there have been some others that have kind of given me pause ketamine
is a hypnotic you know most of the drugs they’re trying out right now are really in my
opinion they’re powerful drugs but a lot of them all of them that I know of have
pretty high addictive potentials too so they make me nervous but you know when you’re
weighing the when you’re going from a harm reduction model that’s not necessarily not
necessarily such the be-all-end-all I guess that’s interesting that you use ketamine in the ER it’s definitely powerful effective stuff and like I said earlier some of the
stuff that some of my clients and some people have seen done experienced I couldn’t even
imagine and you know sometimes for them to actually survive we may need to look at some
of these more intense more powerful drugs PTSD and veteran trauma is not are not my focus
right now and yes marijuana is being experimented with or looked at used whatever however you want
to look at it for PTSD treatment with veterans there’s pretty much not a drug out there they
haven’t tried to throw at it to see well what will this do I believe they were even using
LSD experimentally for a little while too you the VA I mean if you’re interested in this
topic let me see if I could pull that down into here, we go to the National Center
for PTSD US Department of Veterans Affairs has a lot of information if you go for
professionals, it has a ton more information if you can get on get some of your SI CEUs on
demand they do have some free CEUs for PTSD here I’ve never taken any of them but what
I’ve looked at when I’ve looked at like the PowerPoints the presentations and stuff I’m
sure they’re good so if you’re you do focus a lot on PTSD and you can get on-demand CEUs
then this might be a place to get some good free ones aside from DBT are there any other
evidence-based practices for therapy that you’ve seen work best in combination with the
medications cognitive processing therapy when you’re working specifically with veterans
and there is a free course on that too and this one I have gone through
and it’s really awesome CPT dot must seed and here I’ll just put it
into that education and this is a free course oops and here’s the other one ah golly everyone and
embryo does have a lot of research effectiveness with people with PTSD too so yes I would
definitely encourage people to explore all options alrighty everybody I really
appreciate you coming today and sticking with me through this topic and I will see
you on Thursday if you have any questions please feel free to email me or you can
always also send it to support that all CEUs com either way I get it and otherwise I
will see you on Tuesday thanks a bunch if you enjoy this podcast please like and
subscribe either in your podcast player or on YouTube you can attend and participate
in our live webinars with Doctor Snipes by subscribing at all CEUs comm slash
counselor toolbox this episode has been brought to you in part by all CEUs
com providing 24/7 multimedia continuing education and pre-certification training to
counselors therapists and nurses since 2006 used coupon code consular toolbox to get
a 20% discount on your order this monthAs found on YouTube15 Modules Of Intimate Video Training With Dr. Joe Vitale – You’re getting simple and proven steps to unlock the Awakened Millionaire Mindset: giving you a path to MORE money, …
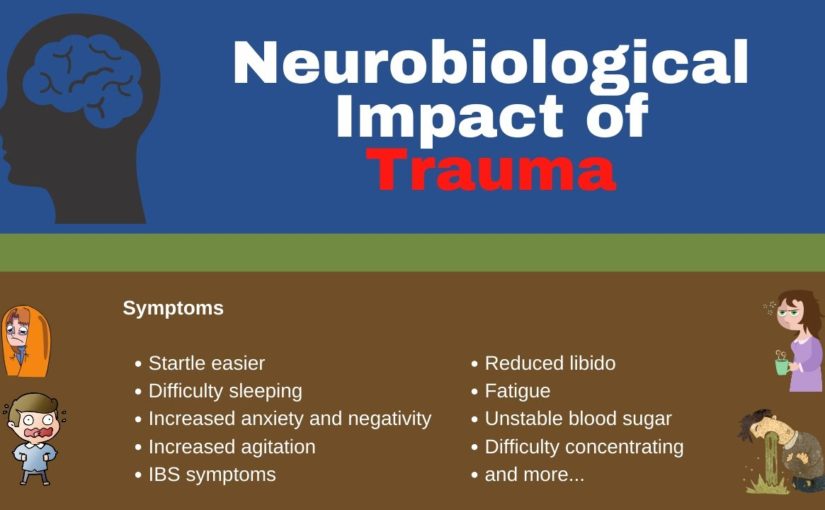

 Earlier today, Steve talked about meaning-making therapy, which is a kind of practical technique for bringing these philosophical ideas to bear in the clinical situation. So the meaning is discovered in three different ways: by creating a work or doing a deed. By experiencing something or encountering someone or by the attitude we take So by creating experiencing or taking an attitude, Frankl says that everything can be taken from Man, but one thing: the last of human freedoms: to choose one’s attitude in any given set of circumstances. This is his famous book Man,’s, Search for Meaning – and I want na point out now that Logotherapy is not a psychology of the mind. It’s not about the Id. The Ego. Psychology internalized objects, relations, developmental stages, and perinatal matrices, It’s not about. Oh, if you look, this is what we find like you, ‘re making a map. It is a therapy of action about the creation of meaning the intention choice and the creation of meaning And Irving. Yalom can’t be left out. American Transcendentalism is a philosophy and a form of literature that had its origins in the 19th century and some ways, lives on today. In the New Age movement, American Transcendentalism holds in the inherent goodness of both human beings and nature. Now this is quite different than Freudian psychology of the late 19th century and 20th century which said that the inherent nature of human beings is filled with steaming, cauldrons of Id and rage and libidinal energy that needs to be modified and modulated to fit with The demands of society, It’s quite different than American Transcendentalism, which says that the individual is pure and it is society that is corrupting American Transcendentalism is an inherently optimistic philosophy. There is a great deal of belief in the self and the self-identity, in creativity and infinite possibilities of the human soul. There’s a belief in spiritual progress and the interconnection of all beings, the immense grandeur of the soul, and that the interior is a source of goodness and wisdom. So I’d like to come back down to Earth now and tell you about the structure of the training program that we have, and this is the structure that we have used just in our last year of training, which is the third cycle of training that We’ve offered.
Earlier today, Steve talked about meaning-making therapy, which is a kind of practical technique for bringing these philosophical ideas to bear in the clinical situation. So the meaning is discovered in three different ways: by creating a work or doing a deed. By experiencing something or encountering someone or by the attitude we take So by creating experiencing or taking an attitude, Frankl says that everything can be taken from Man, but one thing: the last of human freedoms: to choose one’s attitude in any given set of circumstances. This is his famous book Man,’s, Search for Meaning – and I want na point out now that Logotherapy is not a psychology of the mind. It’s not about the Id. The Ego. Psychology internalized objects, relations, developmental stages, and perinatal matrices, It’s not about. Oh, if you look, this is what we find like you, ‘re making a map. It is a therapy of action about the creation of meaning the intention choice and the creation of meaning And Irving. Yalom can’t be left out. American Transcendentalism is a philosophy and a form of literature that had its origins in the 19th century and some ways, lives on today. In the New Age movement, American Transcendentalism holds in the inherent goodness of both human beings and nature. Now this is quite different than Freudian psychology of the late 19th century and 20th century which said that the inherent nature of human beings is filled with steaming, cauldrons of Id and rage and libidinal energy that needs to be modified and modulated to fit with The demands of society, It’s quite different than American Transcendentalism, which says that the individual is pure and it is society that is corrupting American Transcendentalism is an inherently optimistic philosophy. There is a great deal of belief in the self and the self-identity, in creativity and infinite possibilities of the human soul. There’s a belief in spiritual progress and the interconnection of all beings, the immense grandeur of the soul, and that the interior is a source of goodness and wisdom. So I’d like to come back down to Earth now and tell you about the structure of the training program that we have, and this is the structure that we have used just in our last year of training, which is the third cycle of training that We’ve offered.
