Unlimited CEUs for 59 at AllCEUs com welcome everybody. Today,’s, presentation is on dialectical, behavior therapy skills. This presentation is based in part on dialectical, behavior therapy a practical guide by Kelly Koerner. This is one of those books that, if you want to do dialectical therapy as a practice, not just look at some of its tools is a must-read. Then it’s also based in part on dialectical, behavior therapy skills, workbook DBT made simple and DBT for substance abusers, which is an article that was published by Marsha Linehan. So the links to those are in your class, but just give you an idea about sort of the breadth of what we’re going to be looking at today. In the short time that we have together, what we’re going to do is take a look at why DDT was created, we’ll look at understanding emotional regulation, dis-regulation and regulation will identify DBT assumptions about both clients and therapists, and we’ll Explore skills to help clients learn to stress tolerance, emotional regulation, and interpersonal effectiveness. As an aside, we’re taking – or I’ve taken the information from this course and combined it with a bunch of other information to make a six-hour on-demand course. That will be available by the end of the week, but for now, we’re just going to hit the highlights in the 1-hour introduction. So why do we care? Why do we want to learn about DBT skills and DBT tools? Many of our clients, experience emotional dysregulation, or the inability to change or regulate their emotional cues experiences, and responses. Think for a minute about any of your clients, if they’re depressed, if they’re anxious, they’ve got anger management issues, something is going on with their emotional states, or they’re not able to either get unstuck or control their behavioral responses. So they may be engaging in self-injurious, behavior risky, behavior, or addictive behaviors. They’ve tried to change and failed, leaving them helpless and hopeless. In a lot of our clients. We try to fit them in not that we should, but we do try to fit them into this box. If you’re depressed, then we’re going to look at these things, and one thing I hope you get from these webinars is the fact that every single client is different and there is no box that we can put them in and you’re, Like well, then, how can you do group therapy? Group therapy is awesome because you can tailor and that’s, part of the challenge of doing psycho. Educational group therapy is tailoring the tools and helping people tailor the tools to meet their individualized needs, but they can get feedback and they can see how different tools can be modified just a little bit to fit different individual needs and untenable emotional experiences that lead to Self-preservation behaviors such as addiction, you know to kind of numb the pain to give them a distraction, nonsuicidal self-injury. We’re talking about cutting, we’re talking about those sorts of things, and then even those suicidal behaviors. At a certain point, the pain has got to stop, so some people may end up going as far as trying to stop the pain by stopping their existence instead of hurting anyone else. People with emotional dysregulation have high sensitivity, so these people tend to be highly hyper-vigilant. They’re aware of a lot of things that go on now. This was created and I want you to really kind of think about it. It was created as a tool or a protocol to use with people with borderline personality disorder. What do we know about people with BPD? They grew up in really ineffectual environments, so they had to be hyper-vigilant about everything that was going on for their safety and security. So you have someone who, either by nature or by nurture, is hyper-vigilant. These situations have been over-generalized. The dangerous situations have been over-generalized, so the world tends to seem more and dangerous, and out of control, people with emotional dysregulation are easily thrown off kilter because they often have a lot of vulnerabilities. They’re not eating. Well, they’re depressed which is contributing to them not being able to sleep. Well, they can’t focus yadda, we’ve talked about vulnerabilities. One thing that dr Turner talks about is no emotional skin and she likens it to someone who has third-degree burns and every single thing, even the air when it touches it, is just excruciating there’s no middle ground. There’s. No, oh! That’s kind of uncomfortable it’s either not hurting or it’s. Excruciating. People with emotional dysregulation are also highly reactive, so they’re hyper-vigilant. They’re aware of everything that’s going on and then every time something happens that sort of triggers their awareness they jump into this immediate fight or flight reaction. Then they’re slow to de-escalate. So we’re talking about situations in which someone is hyper-vigilant. They’re on edge, maybe because of situations in the past or not. They have this sort of persistent fight or flight or frequent fight or flight reaction. And again, I’ll refer back to our dream fatigue class that talked about how the body can only stand to be all hands on deck for so long before it’s just like dude I give up, and then the sense of depression and helplessness and Apathy starts to set in people who are who have emotional dysregulation, really they’re either like flat and none nonexistent in their emotions. They just can’t even deal with it when they should, or they’re, overly reactive and then the person isn’t in a validating environment. What would be a to some of us on a scale of 1 to 10? As far as how distressing something is it’s, probably like an 8 to somebody with emotional dysregulation, think about a time when you were stressed out or you had a lot of vulnerabilities going on. Maybe you had a new baby at home, so you were, ‘t sleeping and your other kids were acting out. There were just all kinds of stuff going on and you reacted to something with an 8 that everybody else was like that. Doesn’t deserve that. Much of a reaction is that’s it what’s wrong with you, people with emotional dysregulation that’s their environment, all the time, everybody’s looking at them and going what’s wrong with you there? This is not that upsetting. So we need to help people understand that their experience is their experience and it’s not for me to say whether it’s a 2 or an 8. For me, it’s a 2, but let’s look at why it’s an 8 for you. So the emotional reaction – and this is I didn’t – get red eye reduction when I took this picture of bruit but bless his heart. When I got him, he was a rescue and he had such terrible terrible abandonment issues and is so hyper-vigilant. Even to this day, I’ve only had him like four months, but he’s hyper-aware of stimuli and people can be hyper. Aware of stimuli so anytime somebody moves, he’s up, he’s. Looking he’s like. Are you going to leave me alone again when he perceived that something is changing when there was a threat, he goes into all hands on deck and turned into a survival sort of thing and starts acting out? He goes and finds toys and brings them to me. Heaven forbid. We should have to put him out in the garage because we have visitors or something and it’s. You know climate controlled, it’s not like it’s horrible, but he will sit out there and how, until I let him in or go out and tell him it’s going to be okay, now see as a person I’m going. That is not a valid reaction. He’s like totally overreacting to having to spend ten minutes in the garage, whereas from his perspective he’s not overreacting, because in the past when he’s been put in the garage he left out there for days weeks months. Who knows I don’t know his story too. Well, now I use that to kind of highlight the fact that people with emotional dysregulation don’t know what their experience was. What they’re doing is trying to survive. Now they may be trying to survive a situation in their past. You know when there were six and we’re going back to the abandonment discussion that we had the other day, but it’s important to understand that all these things play in together. Something happens and the body’s response system takes in these stimuli and it says it’s dangerous it’s, not dangerous. What do we do with it? The brain decides to fight or flee, and then they go into the survival response with treatment. What we want to do is help people be able to feel that feeling and not have to act on it right away until they can de-escalate some and use a combination of assessing their cognitions and deciding whether their perceptions are based. On the present. The present moment or the past moment so primary invalidation caregivers dismiss emotional reactions as invalid. We just talked about that. The child or person could be mocked or shamed for their emotional response. We have all probably met parents or worked with parents who have children that are highly emotionally reactive, and who tend to get frustrated and overwhelmed by the constant drama that seems to be presented by this child all the time. So the child is often not taught how to self-soothe or de-escalate the parents just like really let it go and go away, which is not helpful because the child doesn’t learn how to deal with it. The child is not taught mindfulness to figure out okay, what’s causing this, and the child is not taught effective cognitive processing in most situations in validating environments, if the child gets upset, even if it seems to be disproportional to whatever the event was, the caregiver Will take the child in and say? Okay, I hear you’re upset right now, let’s talk about it and we’ll walk the child through, maybe not thinking about it, but just being a good parent walks. The child, through this de-escalation process and the cognitive processing of secondary trauma or invalidation, is, and I’m putting this in here. Coping skills can be overwhelmed by trauma or intense stress, leading to this high alert raw status. Think about the people who were survivors of Hurricane Katrina or Hurricane Andrew. I come from Florida, so I think hurricanes, but any big event that is ongoing enduring, and distressful at a certain point. You’re on your last nerve, so anything could precipitate sort of a crisis. Many people don’t receive the necessary support during these times and may be shamed for being weak or needy. Sometimes nobody can cope and everybody’s kind of decompensating. At once, which is a lot of what we saw with Katrina but other times there may be people that are functioning just fine and they don’t understand why some other people are 39, t coping just fine, and they see that as abnormal and want to distance themselves from it, it’s important for us to communicate to people because we already noticed that crisis is a normal response to an abnormal event. What was abnormal, though, is it this particular incident? Maybe, or is it the fact that this particular incident kind of was the straw that broke the camel’s back on a whole chain of incidents leading up to it that was abnormal? What caused this person? Excessive stress I was talking to a woman the other day who, in the past six years, has had half a dozen significant losses and I’m just like wow. You know that that’s pretty intense to have all those and she’s, also starting her practice and everything else. Right now – and I’m – just like oh my gosh – I can’t imagine the amount of stress this woman is – going through most humans, aren’t inherently prepared to deal with the crisis alone. We’re kind of group sort of people. We rely on other people, so if we have this reaction and it’s judged to be disproportionate and people kind of distance themselves from us, because they see us as abnormal or dysfunctional, then we lose any social support that might have been able to serve as A buffer which just kind of in turn, feeds back and exacerbates the sense of hopelessness, helplessness, and isolation. What precipitates a crisis may vary between people based on pre, existing stress or mental health issues, and it also may vary with the same person longitudinally across time. What may be overwhelming today – maybe not may not be overwhelming six months from now, because all of those prior stressors that I’m dealing with right now may have had time to kind of work themselves out. So we must help people understand that their reaction is their reaction and let’s just go from there. Let’s not say it’s bad or is disproportionate or it’s whatever it just is so the result of this sort of unpredictable reactivity results in frantic efforts to numb withdraw or protect. I need to numb the feelings because I can’t take this kind of pain. If you’ve ever had a burn that’s had to be cleaned or even an open wound that’s had to be cleaned out. You know that’s pretty excruciating so thinking in terms of that, you can see why people would want to kind of get a little novocaine withdrawal if this support system is invalidating, that has extra pain and that’s excruciating to be rejected. On top of everything else, so a lot of times, people withdraw which eliminates any opportunity for social support, and it also exacerbates this sense of rejection, and they do this to protect themselves. People learn who they are in invalidating environments. They learn who they are and how they are resulting in rejection, so they avoid threats. They avoid putting themselves out there. They avoid making relationships because they’re afraid of rejection and they avoid thoughts and feelings and sensations that may lead to invalidation. I don’t want to feel these things because then if I do and I communicate them, you may tell me I’m wrong. Okay, we’ve laid the groundwork. Now we see where this is a problem. So what do we do about it? Well, the first thing we want to do is look at some of the DBT assumptions about clients. Clients are doing the best they can given the tools they have at this present point in time, and I truly believe that clients want to improve themselves. Wouldn’t be in your office if they didn’t want to improve for one reason or another. It may be an involuntary referral and they want there’s a means to end there. They are in your office because they have hope that something can change and it will benefit them. They cannot fail at DBT if they go through dialectical behavior therapy, the protocol and it fails, then the protocol failed them or we as clinicians, fail to implement it correctly. Now, today, again, we’re talking just about tools that are present in DBT, not how to do dialectical, behavioral therapy. The evidence-based practice wants to make that very clear clients are existing in what is for them an unbearable state. This pain has got to stop. They need to learn new behaviors in all contexts, not just at work, not just in their relationships, but they need to learn how to function and deal with life on life’s terms in all contexts, so they can go to the grocery store they can get In a traffic jam, they can be in a crowded Airport and not feel like the walls are closing in on them. Clients are not responsible for all of their problems. We know this some things they had no control over are causing problems for them, but they are responsible for all of their solutions, and we’re going to talk about the four options for problem-solving in a few minutes, but they are responsible. They choose to do something and clients need to be motivated to change motivation, choosing the more rewarding option out of the available options. Well, yeah that whatever they’re doing right now is the most rewarding option they have available in their toolbox. So we’re going to give them new tools, but then we need to teach them how to make those tools effective. If you just hand me a jigsaw and say, okay go about woodworking and whatever I’m, not a woodworker, but I’m not going to know what to do with that. So I may go back to using my circular saw or whatever the case may be, which may be very clunky. We need to help clients learn how to use these new tools, so it’s more rewarding to use those than those old behaviors. They just numbed out the pain or distracted them assumptions about therapists, clarity, precision, and compassion are of the utmost importance. We need to be clear with our clients about what’s going on. Let’s not speak in generalities. We want to try to avoid some of the Socratic questions that we would normally do. We want to be clear about what we’re getting at and what we want them to look at. We need to be precise. Do we need to not say well what is it last week that caused all the problems in your relationships? Well, if they had four different fights that’s four different things we need to look at, we need to be precise to identify all of the things that trigger and we’re going to talk about behavior chains in a few minutes. So we need to be precise. We also need to be compassionate, even if we don’t agree, or we think that the reaction was disproportionate, putting ourselves in their mind in their place in their raw state. We need to be compassionate and go okay, you survived it, you did the best, you could let’s take a look at what might have caused that. Why you made the choices you did and what you might choose better next time. The therapeutic relationship is between equals, DBT or therapists can fail to achieve the desired outcome, but the client can’t fail and therapists who treat patients with pervasive emotional dysregulation needs support we need to remember that patients who are always in crisis by their very nature, it’s, exhausting because they’re always in crisis, which means we are responding in a crisis manner, not that we need to get all upset and worked up because that’s just modeling the wrong thing. But there is a lot of energy that it takes for us to use the DBT tools for us to model the DBT tools and for us to help work. The client is out of their emotional state into one where they can use their wise mind. So the first step is core mindfulness. Until they figure out what’s going on, they can’t fix it, so we want to help them integrate their rational mind they’re cognitive. This is what happened factual mind with their emotional mind. This is what it felt like in the wise mind, so you can take the facts. You can take your feelings and you can say with what I know and what I felt. What would be the best interpretation of this or the correct one for me? Interpretation of this event at this point, and what can I do about it? One of the things DBT talks about is the fact that truth is sort of subjective. What is true for one person may not be the truth for the other person, because we’ve all had different experiences, but we need to help people not underreact and stay. In that cognitive mind, if you’re a star, trek fan, think data um. He was the AI that was kind of human-robot sort of thing or, and we also don’t – want people to act in their emotional mind, acting solely based on feelings and trying to make feelings facts because feelings aren’t facts. They’re feelings, so we want to help them integrate these two things, and that is more difficult and it sounds like it takes time. Mindfulness is using effective, nonjudgmental observation and description of experiences, those thoughts, and feelings, and identifying what’s the objective evidence for and against what’s going on right here, how I’m feeling what is all the evidence. Let’s look at the big picture, not just one little aspect of it, and what are my feelings about this event? Getting in touch with what’s going on inside their mind and inside their body is going to be one of the first steps. So I talked about those four options: when there’s a problem, you have four options. You can tolerate it, grit your teeth, and Barratt there. Sometimes you just can’t do anything about it. Traffic jams probably can’t do much of anything about it. Change your beliefs about the event. Instead of seeing a traffic jam as a waste of time and just a complete pain in your butt, you can see it is a time to check voicemail and maybe return. Some phone calls are productive, make it billable, and you can solve the problem or change the situation, while you’re in a traffic jam and stopped, of course, looking at Google Maps to figure out where the next exit is so that you can get off. So you can change that situation or you can choose to just stay miserable and choosing to stay miserable is a valid choice. When clients make these decisions, we need to look at them. Why was that? Whatever their option was? Why was that option more rewarding than all the others? Why is it more rewarding sometimes to stay miserable for some people that’s what they know and they’re afraid if they feel happy, then they may get disappointed and end up feeling sadder than they already do now? Some people tolerate the problem because it’s what they know and change is hard and they would rather just tolerate it and deal with it and suck it up than have to muster up the energy to try to change whatever’s going on. So again we want to look and ask them or ask ourselves, maybe because they may not know right away the choice that you made. Why was it more rewarding? Why did you choose that over the other three options, distress, and tolerance we’re going to talk about a lot of acronyms here acronyms are really important in DBT because it helps clients have sort of a drop back and punt. There are some worksheets. There are lots of worksheets online for DBT but the acronyms we’re going to hit here are going to be some of the highlights that are going to be important for you to remember tip temperature. So you’re tipping your physiological balance now temperature. I’m not necessarily advocating for this. You don’t want to do it. If you’ve got a heart condition. You don’t want to suggest it to clients that have a history of child abuse, especially anything that involved drowning. So this one’s a little tricky one of the things I suggest to some of my clients instead of this is holding on to ice cubes. But the suggestion in the book holds your breath. Dunk your face in for as long as you can hold your breath into a sink full of ice water, then come up. Exhale, inhale and dunk, again repeat as many times as you need until you feel calmer. Well, guess what we’ve talked about combat breathing. If you are slowing your breathing, which you do, if you’re holding your breath, your heart rate is naturally going to slow. When your heart rate slows down your brain says: oh the threats going away, yippee yay, I can call off the dogs. There are other ways to slow down your breathing. Besides necessarily dunking your dunking, your head holding ice cubes is one of the reasons that that can be helpful. Instead of cutting the person’s focus, it’s a distracting technique. The person focuses on the pain because it is painful to hold on to ice cubes for a long time, instead of cutting themselves, but it also gives their body something to focus on to go. Oh, my heart rate is up because there’s a pain when the pain goes away. I can make my heart rate go down, so we’re redirecting the brain to go. Oh, this is why the heart rates are up it’s, not because there’s emotional distress, it’s because of extreme physical pain. Intense exercise increases body temperature, but it also increases the heart rate when you’re sitting still and your heart rate is 120 beats a minute because you are in a panic attack or a state of panic. It’s very, very uncomfortable and your mind is going. I don’t understand you, ‘re not moving. Why is the heart racing when you start exercising, which is why walking and getting those big muscles moving often helps? Then the body gets less confused. It’s, like Oh heart rates, beating fast, because the body is moving score, got it so when the person stops moving, the heart rate starts to go down, and this is true, even if you’re walking around. If you take a client out to walk when they’re upset – and you are talking about whatever the distressing thing is – I have found without exception.

When they come back inside, they can start to calm down a little bit more and their heart rate naturally starts to go down when they stop their physical exercise and then progressive relaxation. You’re going to move from head to toe or toe to head. Whatever you prefer but head to toes, usually how we do it focusing on muscles focusing on breathing slowing, breathing relaxing muscles forcing the body to relax. So this addresses physiological arousal, so the temperature, intense exercise, and progressive relaxation. All of these serve as an ability serve the function of distracting the person from whatever cognitively or inter psychically wants to say, is going on, and all of these either explain to the brain why the heart rate is going so fast or Help reduce the heart rate, so you know there’s something to be said for them. The important thing is for you to brainstorm with your clients when you get physiologically aroused when you get upset, and you are just your hands – are shaking your palms are sweating. You’re breathing fast, and your heart rate going fast. How do you calm yourself down what works for you and we’re back to bruit again? Another acronym is accepted to distract when there’s emotional turmoil, so you can kind of let that adrenaline surge go because you have that initial fight or flight reaction and then the body kind of goes. Alright, let’s reassess and see if there’s still a threat, get involved in activities that will help you distract yourself from whatever’s going on when kids get upset. You know if they’re getting stressed out because they’re sitting in the lobby and the doctor’s office, and they know they’re going to get a chhoti. We give them something to do. We read a book, we talk we play because then they’re not focusing on the fact that they’re going to get a shot, contributing to the welfare of others. Do something nice for someone to volunteer. Do something productive that gets. If you are focused on someone else, compare yourself to others who are doing less well, that doesn’t work for everybody. You can also compare yourself in the present to your old self and focus on how much better you’re doing now compared to what you were doing six months ago, this doesn’t always work. You know these are options. Not everyone is going to work for every person, emotions do the opposite. If you’re feeling really sad get a comedian, get it to go to YouTube, and Google a comedian and watch a skit or two or ten, so you’re doing something that makes you laugh. That makes you happy to sing. Silly songs, dude silly dances go out and there’s very little. I find it more amusing than just listening to a baby laugh. If I’m having a really bad day, I will find those stupid videos of babies laughing at paper tearing if you can’t help, but laugh with them pushing away build an imaginary wall between yourself in the situation. Imagine yourself pushing away the situation with all your might or blocking the situation in your mind, and each time it comes up, tell yourself to tell it to go away. So if you start thinking about something that is particularly hurtful as soon as it comes into your mind and it comes into your awareness go no, I am NOT going to think about that right now. Thoughts counting some people count to ten, a hundred whatever it takes to get through that initial rush. Some people sing for me. I think I’ve shared before I have this irrational fear of bridges, but so, whenever I Drive over a bridge I sing, and usually, it’s, not songs on the radio. Usually, it’s songs. I used to sing to my kids. I’ll sing the ABCs something that doesn’t require a whole lot of cognitive interaction because I’m doing pretty good just to get over the bridge. And yes, I know I should be over it, but I’m not and that’s just the way it is the 10 game. I like this one think of 10 things that you like the smell of think of 10 green things. Think of 10 things you see where we’re going with this, and you can incorporate all the different senses with it. If you go through multiple iterations of it 10 things that you smelled yesterday, 10 things that you see right now, 10 things that you hear when you’re on your way to work. This helps people focus on something other than what’s going on. Here the 5 4 3 2 1 game is sort of similar to the 10 things game, identify 5 things. You see, 4 things you smell, 3, things that you can touch and follow down. Sensations like I talked about on the last slide. Sensations can help distract you from what’s going on until you have a chance to kind of get through that initial adrenaline rush, cold, holding ice, cubes, rubber band – and I don’t like this one. But some people do they put a rubber band on their arm and every time they start to perseverate on a negative thought. They snap its smells and find some good smells. Some smells bring back good memories, smells that you like. Maybe it’s roses: maybe it’s a purse-specific perfume. Maybe you just go to Walmart and start smelling all the air fresheners. Whatever makes you happy, I do suggest avoiding taste, because if you start using taste as distress tolerance, then you start moving toward emotional eating. I’ve seen it happen, so I would avoid that for most people, but if they just desperately want to go there, then you know we’re going to go there because they are choosing how to distract from their cognitive or intrapsychic. Sensations improve at the moment. Imagery goes to your happy place. Whatever your happy place is meaning find an alternate, meaning for what’s going on now. This can be Linehan refers to it as making lemonade. We all know how to do that. We don’t we’re, not necessarily the best at it, but try to make lemons. I try to look for the optimistic meaning in whatever it is prayer. Now, even if someone is not religious, they can be using radical acceptance. Accepting it is what it is and not trying to change it, just putting it out there for the universe, relaxation is always good to relax one thing at a time and this isn’t focusing on one problem at a time. This is focusing on something we’re talking about distress, tolerance, and improving the moment so focus on one thing, like your breathing: get your breath and calm down once your breathing calmed down. If you need to focus on something else, then move to. Maybe the tension in your neck. Maybe you need to lower your shoulders and release the tension in your neck, focusing on physiological things and focusing on other senses. Besides, that abstract stuff that’s in your head and your emotions can help people tolerate the distress until they can think more clearly vacation takes a timeout. Sometimes you just need to get away from it. For a few minutes, we’ve had time at work. I’m sure we all have where you’ve just been like. You know what I’m done and you lock your computer screen. You get up, you walk out of the building, and none of its clients are in there, but you walk out of the building and do a couple of laps around the campus and then you’re like okay. I can deal with this again just clear your head before you try to tackle whatever it is, an encouragement providing yourself, because you can’t necessarily rely on anyone else. Positive and calming self-talk now back to those stupid, memes and videos that I love to death there’s, one has a kitten on a laundry wire and it says: hang in there, I love having those things on screensavers. It’s, juvenile, maybe but whatever it makes me happy, and it reminds me you know even when I’m, not in a state of emotional distress. It reminds me all right keep on hanging in there. You got it and it’s got an all-factor too. So I always like anything with an all factor: the goals of emotional regulation. So once you’ve tolerated this distress, you’ve gotten through that initial surge. That initial, I cannot take this pain or upset. Then we need to move into emotional regulation, help people identify labels, understand their emotions and the functions of those emotions, decrease unwanted emotional responses and decrease emotional vulnerabilities. So what they’re going to do is identify and label emotions and their functions. I’m scared. Okay, you 39. Re scared. Tell me why what’s the function of you being scared? What do you want to do, and what do you think is causing this scared? 39. No self-awareness through questioning, like that through talking it out, people will start to understand where their emotional reactions are coming from and they can choose whether or not to follow up with it a behavior. What I guess I didn’t put in a behavior train analysis is the way you can go about helping people work through that and that’s a couple more slides cop. We want to police our thoughts and check the facts. Look at doing opposite actions. If you want to hurt yourself, look at being kind to yourself, if you want to run, maybe you need to look at staying and then look at the problem. Solving reduced vulnerability through the ABC p accumulate. The positives, remember, vulnerabilities, are those situations that happen leading up to whatever the distress is. Those are the things that make you more likely to be irritable, overwhelmed angrily depressed get sad about anything. Instead of not so, we want to eliminate those vulnerabilities or reduce them. As much as possible, so we’re going to accumulate positive gratitude, journals pictures if well, everybody has things in their life that they care about. Have those on your phone in you know little picture galleries that have them as your screen. Savers have reminders around about it. Why you get up in the morning builds mastery, so you have mastery of the skills you need to deal with emotional distress and upset cope ahead of time plan for distressing situations. If you’re getting ready to go in for an annual evaluation and those things stress you out to no end rehearse, it ahead of time plan on coping ahead of time, and figure out how you’re going to react. If it goes bad figure out how you’re going to react, if it goes good figure out how you’re going to cope and physical vulnerability prevention, maintain your health, chronic pain, chemical, chemical imbalances, hormonal imbalances, those can all cause vulnerabilities or set you up. Make you predisposed to feeling like something’s at eight when it’s only two get plenty of sleep when we’re sleep deprived, is a whole lot harder to deal with life on life 39. S terms and exercise. Exercise is a great way of releasing or using up some of that stress energy that you release during the day. Behavior chain analysis. The first thing you do and a strict behaviorist will have slightly different explanations for how to do this, but just bear with me here: name the behavior reaction. What happened now, if you’re thinking back to the ABCs, this is going to be your C. Your consequence, what happened identifying the prompting event ABC is, that would be the what was the activating event now. This is where it differs a little bit. Then we want to look at the behavioral links, so you had the activating event, and then there was this reaction and in between, there were um automatic beliefs, and we have that there. We have thoughts, but there were also sensations events, and feelings between what happened and your reaction. What sensations did you feel? Did you get flushed? Did you feel nervous? Did you feel scared? Did you feel sad? Did you have a twinge of something? What feelings were there and what events happened? Did you act out in a certain way? Did you scream? Did you yell about what happened? Because these are all things that are going to go into what ultimately ended up being the behavioral reaction, then I want to look at the short-term positive and negative effects of what you did. The behavior of the reaction. If you started screaming and throwing things okay, you did what was the short-term positive effect of that? What was the benefit of that? Because that was what you chose, which means it was likely the most beneficial response you could come up with in your highly emotionally charged mind then. So what were the benefits and what? With immediate short-term negatives and then looking at the positive and negative long-term effects in the long term, if you react to this upset by screaming and throwing things what’s the impact going to be, are there any positive impacts? Are there any potential positive effects of this and a lot of times it’s? No, but we want to ask the question just in case there are because some people will have a positive and we need to address that this is sort of. If you go back to motivational interviewing what we think about when we’re talking about decisional balance, exercises address the problematic links with skills. If some sensations or actions exacerbated the distress, then we need to look at distress and tolerance. If all of a sudden you had this immediate panic reaction and you couldn’t breathe, we need to work on distress, and tolerance skills, so you don’t go to that point where you are just for lack of a better phrase in a tizzy thoughts and Feelings if your thoughts get negative and start racing and your feelings are negative and anxious and worried and all those negative words we want to look at emotional regulation. You know if you can get through it, where you get through that initial rush and you’re still having these getting stuck in the negativity. Then we want to look at emotional regulation most of the time we’re going to look at both of them and then the third component, once we’ve learned how to get through the initial flood, the initial all-hands-on-deck call, and then people Have learned to regulate their emotions and identify helpful responses, and instead of talking about good and bad, we want to talk about helpful and less helpful responses. Then we need to look at interpersonal effectiveness and how to interact with other people to make that validating environment exist. So we want to start with interpersonal and intrapersonal if you will be effective with yourself and then move to others describe what’s going on assess how you’re feeling what your reactions are, and what the best next step is asserting. Your choice reinforces the good things. Be mindful appear confident and willing to negotiate, and yes sometimes we have to negotiate with ourselves because there’s something that we want to do right now – and this is very true – with people with addictions a lot of times – they want to use. They know the long-term consequences of use are not where they want to be, so they have to negotiate with themselves to say alright. I want to do this right now, but I’m going to choose a different option in their relationship with others. We want to encourage them to give me gently instead of critically, and harshly, which a lot of times is what they’ve gotten all of their life, being gentle with other people, accepting them where they are modeling how they want to be treated, be interested in What other people have to offer, what other people have to say and what’s going on with them? A lot of people with emotional dysregulation can’t handle their own life on life’s terms. They can’t even begin to handle anybody else.’s stuff, so a lot of times they appear disinterested, validate other people and their experiences, and have an easy manner. You know sometimes we get too intense and if everything in your world is either a zero or a ten, it’s easy to be intense. About everything, as they develop emotional regulation, things will be different. You know they’ll have fours and fives in there, but practicing that not being intense and over the top about everything, and then in their relationship with the self, be fast, be fair with themselves, not judgmental just fair, avoid apologies, stick to values and be truthful. 12-step recovery step, one starts with honesty, being honest with yourself step two. We start talking about hope and faith, which is sticking with values and being fair to oneself. Being compassionate comes couple more steps down that’s not hard or not harmful. For any of our clients to teach them to be fair, to be kind to themselves, and to be honest with themselves and others. So how does treatment progress when we’re talking about dialectical, behavior therapy as an evidence-based practice stage? One is safety. We want people to move from behavioral disk control to behavioral control. We don’t want people getting a phone call, maybe a significant other has to back out on a weekend trip which was someone with behavioral disk control could send them into a state where they are self-injuring. So we want to make sure that they have the skills to not self-harm, and you know you can’t just say. Well, you can’t cut the person’s like okay, so finish, what am I going to do? Instead? If I can’t cut, if I knew how to do something else, I’d be doing it right now. We need to help them increase their self-care behaviors instead of cutting. What can you do, I’ve talked before about some of the interventions I’ve used with some of my clients that have self-harmed. It’s not ideal. It’s not where you want to end up, but moving from self-harm, too, like I said, holding ice cubes or using a ballpoint pen to draw on yourself is preferable to cutting yourself. So we want to look at small steps, not going from. You know five or six self-harm episodes a week to nothing. You’re setting yourself and your client up for failure. We want to reduce the intensity of the self-harm, so they’re not breaking the skin, so they’re not damaging themselves decrease therapy interfering behaviors what we typically call resistance and that can be showing up late that can be always coming in and trying to derail therapy sessions, it can be being bossy, it can be being reserved whatever it is that’s interfering with the therapeutic process. It’s important to understand that therapy-interfering behaviors can be exhibited on the part of the counselor too. If the client is experiencing a lot of emotional discount role, sometimes counselors will start being late to sessions and will start forgetting to review the chart before they go in and remember what homework was assigned will start forgetting to do things. So we need to make sure that both the counselor and the client are engaging in motivating therapy participatory behaviors. We want to increase the quality of life, and behaviors and decrease the quality of life-interfering behaviors. So if they’re engaging in addictions, if they’re, not sleeping if they’re, changed smoking if they are and again these are things when we look at the priority list, my main focus at first is going to be on self-harm. You know I don’t want them to be engaging in those behaviors, and then we’re going to start looking at the other things that create vulnerabilities that make them more likely to be unhappy or to be reactive in situations that would make them unhappy. We’re going to increase behavioral skills, core mindfulness, and accurate awareness, encouraging clients, not just when they’re upset, but to engage in mindfulness scans body scans, four or five times a day. So they know where they are and they know if they are starting to feel vulnerable. If they’re, it feeling exhausted all of a sudden. If they’re feeling foggy, then they know to be kind to themselves: distress, and tolerance. We talked about those skills, interpersonal effectiveness talked about those skills, emotional regulation, and active problem-solving. So these are all going to be introduced in stage one, but they’re introduced. The client has been using their old behaviors for a lot longer than stage 1 is ever going to last. So we need to remember that we have to help clients strengthen these behaviors, remember to use them if they use them at first, one out of every five times as one more time than they were using them. Last week let’s focus on the positive forward movement and not on what we think they should have done. We don’t want to set goals that are going to set them up for failure in stage two. We want to help clients, moderate emotions from excruciating and uncontrollable to modulated and emotional um. We want to feel feelings. Well, I mean, theoretically, we do so. We don’t want people to completely numb out and become robots, but we also don’t want every single emotional experience to be like debriding. For a third-degree wound, we want something in between. We need to help them decrease intrusive symptoms, like flashbacks memories, and hecklers, the things that created the situation where they feel unlovable and unacceptable for who they are. We want to decrease avoidance of emotions, and I know that sounds kind of counterintuitive to increasing emotional awareness. Again, we don’t want them to be numb. We want them to feel because if they feel, then they can choose how to act and how to react. Decreased withdrawal increases exposure to live a lot of times, clients with emotional dysregulation have withdrawn because they don’t want to be rejected so they don’t go out with friends. They don’t experience life on life’s terms. They just sit in front of the television watching Netflix. We want to decrease self-invalidation and help them understand that their experiences are their experiences and they’re not right or wrong. Their choices may be helpful or less helpful, but at any point in time that is their best as well as they can see their best options for survival. So let’s not be critical. I’m just happy you’re still here and we want to reduce mood dependency of behaviors part of this process. We’re going to teach people how to create SMART goals that are specific, measurable, achievable, realistic, and time-limited SMART goals and make sure they’re successful by validating and teaching them to self-validate, encouraging them to imagine the possibilities when you’re successful When you accomplish this goal, what’s going to be different? How awesome will it be to encourage them to take small steps, not all or nothing? You know we want to get get rid of the dichotomy’s small steps towards recovery and applaud themselves for even trying to encourage them to lighten their load and get rid of stuff that they don’t need to be stressing over right now. You know maybe now’s not the time to start remodeling the house and then sweeten the pot and encourage clients to provide themselves with rewards for the successful completion of a goal, maybe getting through an entire week or for some clients even an entire day without self-injury. I encourage you to practice these skills yourself because you’ll see how much we don’t do and how helpful these skills can be, but it also gives you more insight into two ways to help explain thanks to clients and help them apply. These tools to themselves think about which skills you’ve used that were helpful or skills you could have used. That would have been helpful in the past week for you because you’re going to ask the clients to do this. So let’s do it for ourselves, so we can put ourselves in their position and think about which skills might have been helpful for a client that you’ve worked with in the past week. Many disorders involve some amount of emotional dysregulation. That dysregulation can be caused by high sensitivity and reactivity due to innate characteristics and poor environmental fit or external traumas and lack of support, or both DBT seeks, first to help the person replace self-defeating behaviors with self-care behaviors, and then moves toward emotional regulation and Interpersonal effectiveness to help people develop the support system and learn how to feel feelings, including the good ones. A variety of tools are imparted to clients to help them set SMART goals, identify and understand, emotions and their functions, decrease, unwanted, emotional and behavioral responses, and develop a more effective, compassionate, and supportive relationship with themselves and others. Finally, remember that not every tool is going to work for every person it takes some experimentation, so prepare your clients for that. Otherwise, if they try something and it doesn’t work, they’re going to feel rejected and validated and like failures. Again, it’s a process to work together to help them figure out how they can start interfacing with life and integrate the two dichotomies of thought and emotion to make wise choices to help them live happier and healthier. .
As found on YouTubeHi, My name is James Gordon 👻🗯 I’m going to share with you the system I used to permanently cure the depression that I struggled with for over 20 years. My approach is going to teach you how to get to the root of your struggle with depression, with NO drugs and NO expensive and endless therapy sessions. If you’re ready to get on the path to finally overcome your depression, I invite you to keep reading…
 ☃in 5-10 Minutes A Day Using Automation Software and our Time-Tested Strategy See How Your New Site Can Be Live In Just 27 Seconds From Now!
☃in 5-10 Minutes A Day Using Automation Software and our Time-Tested Strategy See How Your New Site Can Be Live In Just 27 Seconds From Now!



 If you will, I don’t keep them in the house, but I will allow myself occasionally to buy a small snack-size pack of M Ms, when I’m out or I will get a regular-size pack and I’ll share it with my daughter, so I’m not restricting it.I’m not saying I can never M. Ms again, I’m just not making it available to myself when I might have some unrestricted time, try to avoid buying a bunch of comfort foods and keeping them around the house, and when you’ve got kids when you’ve got family, it’s not entirely possible, usually to not have some of that stuff around but try to avoid having the things that you particularly used for comfort, because if it’s not readily available, then you’ve got to focus on guess what dealing with the emotions.Instead of stuffing them with food, try not to go too long without eating.Like I said earlier, if you go too long, then by the time you get to the food, your blood, Sugar,’s low and you’re just shoveling it as fast as you can initially distract.If you know that you’re getting you’re eating and you’re, like I’m – really not hungry, but I want to eat, take a bath, take a walk, call a friend, heaven forbid get on Facebook.Whatever it is, you can do to distract yourself for 10 or 15 minutes if, after 10 or 15 minutes, you’re still going, I want whatever it is, then you can decide what to do about it.Then, most of the time when people stop and go, I’m not hungry.Let me distract myself.They get caught up in that distraction and before they know it, they’ve forgotten about the craving, and identify the emotions.If you know that you’re not hungry, but you want to eat, then say: okay, what’s going on what’s going on with me? It doesn’t mean that the person is never going to eat when, when they’re upset, because a lot of people do, and is it the end of the world, probably not necessary if they can start reducing the frequency of times that they eat.In response to emotional distress that’s, what we want, we want to progress, not perfect if it’s, depression, what’s causing them to feel hopeless or helpless right now, if it’s, stress, anxiety, or anger, remember our big kind of lump together stuff. What are they stressing out about? Do they feel like they’re overwhelmed? Are they afraid of failure, rejection, and loss of control of the unknown? We’ve gone through those things.We want them to identify what’s going on with them, and then they can make better choices about how to deal with it.So general coping helps them develop, alternate ways of coping with distress.Distract we’ve, already kind of gone over that one.I encourage people – and you know it’s – one of those DBT things – that a lot of therapists encourage their clients to keep a list of things.They can do to distract themselves because it’s not always practical to get up and go on a walk.If you’re at work or it’s, you know two in the morning.So what else can you do to distract yourself? Talk it out with a friend with yourself with your dog? Sometimes you just got to get it out.People who are more auditory will prefer talking it out as opposed to journaling it now.If they talk it out with themselves, they can record it if they want to, or sometimes it’s just better to have a dialogue with themself. If it worked for Freud, it can work for other people journaling.If your clients are inclined to journal, encourage them to write it down.Sometimes just getting stuff out of your head and onto paper will help the feelings dissipate a little bit.So you’re not mulling them over and obsessing over them and getting stuck in those thoughts and feelings.Additionally, while you’re distracted talking it out or journaling, this is also your break.Your stop between the urge and the behavior make a pro and con list of the de-stress, not the eating whatever it is, that’s stressing you out and how can you fix it or what are the pros of this situation and what are the downsides To this situation, encourage them to focus on the positive.You know.If something stressing you out at work, you know you’ve got a big meeting coming up or something you don’t want to do or what it is.You can get stuck on focusing on that or you can focus on the positive that you do have a job.That meeting only comes around once a month. You can it’s time you don’t have to be doing paperwork whatever the pros are for that person encourage them to focus on the positive.If you’re distressed because of some kind of a failure or perceived failure, figure out what you learned from it, whether it was a relationship failure, or maybe you learned what not to do in a relationship anymore. Maybe you learned things that you may have ignored.Maybe you learned what you should have done instead, but how can it be a learning opportunity, instead of somewhere to stay stuck and finally, if something’s making you upset if something’s causing anxiety, depression, hopelessness, helplessness, whatever the negative feeling figure out.If it’s worth your energy to get stuck here, is it worth the turmoil? Is it worth you know having to pacify yourself with food or whatever? It is a lot of times people say you know what now it’s, just it’s, not even worth my effort.It’s not worth moving me away from my goals, because my goal is to stop emotional eating.My goal is to eat for hunger, so I can go to dinner with people and feel comfortable.I can be at a party where there’s a buffet and not feel stressed out that I’m going to go and eat half the stuff on the buffet that’s my goal so is holding on to whatever this de-stress is getting me Closer to being able to do those things and generally the answer:’s no develop alternate ways of coping with the stress the ABCs, the a is the activating event.What is stressing you out and what’s causing the de-stress C is the emotional reaction.Angry depressed stressed, whatever be: are your behaviors? What behaviors or B are your beliefs? Sorry, what are the beliefs that are in there that may need to be addressed? What kind of things are you telling yourself, and, and how can you counter them? Cognitively eliminate your vulnerabilities.You knew we couldn’t get through a presentation without talking about vulnerabilities. If someone is well-rested.Well, the fed has a good social support network, not stretch timewise.Then it will be easier to deal with stress or stressors when they come your way.You’ll have more energy to deal with it, so there won’t be this overwhelming feeling of I just want to bury my head in a jar of peanut butter, be compassionate with yourself.Some days, you know you’re, just going to feel anxious.You’re going to feel depressed.You’re going to get angry.You can beat yourself up over it and you know a lot of people do.Is that the best use of your energy or can you be compassionate? Can you learn from it? Can you give yourself a break and go? You know what I’m having a bad day today and that’s okay, I’m not going to unpack and stay here, but I’m not going to fight.It either helps clients learn how to urge surf help. They understand that, just like a panic attack just like a wave just like a lot of other things in life, it will come, it will crest and it will go out again, so they can sort of identify where they are on the energy of that Urge other tools people can use close the kitchen once I have the kitchen cleaned and you know all the dishes are done and it looks pretty.I hate going in there and finding dishes in the sink again now I’ve got teenagers, so we always have dishes in the sink.But before I had children, you know at seven o’clock.I finished all the dishes and closed the kitchen, and that would be enough motivation for me to not go in there and at least not use plates and stuff to eat.So if we’re saying that we’re going to only eat using utensils plates and sitting and all that stuff that we already talked about, then once you close the kitchen, you’re not going back in, there turn off the light.That also helps so you’re not being attracted to the pretty lights, and you know all the goodies that are in the kitchen to brush your teeth.This is something my grandmother used to do and it works.There’s some research behind it.Minty flavors reduce our appetite.So if you brush your teeth, you get all the other flavors out of your mouth and it reduces your urges to eat because it again it’s clean and fresh. And do you really want to brush your teeth again, and meditate, sometimes just getting in a space where you’re, not obsessing about anything, can help people get past that urge to self-soothe by eating a CT for emotional eating.What am I feeling or thinking about what’s going on with me right now? What is important to me? So if I am thinking I want to eat, I want to you know just dive into this jar of peanut butter, and then I think about what’s important to me.Is it important to me to get control of this? Is it important to me to you know, be able to fit into my clothes in six months or not? So what is it in? What way is controlling my eating habits and eliminating emotional eating important to me, and how does that get me closer to other things that are important to me, and what other things could I do? That would get me closer to my goals.So if the goal is to have improved relationships, be able to feel more comfortable around food reduce the stress around going out to eat, and just around food in general, what else can you do when you are stressed out? Somebody also suggested that adding a blue light in the refrigerator decreases the appeal of foods, which is interesting because yellow red and orange, and browns, I think Pizza Hut – are all foods that increase people’s, hunger and desire to eat.But blue is just a completely different primary color, and adding a blue hue seems like that would be effective, so cool thanks for that.Little tidbit there holiday help, and you know we’re coming into the holidays.So I’ve got to bring that up at every single glass and choose lower-calorie foods.If you tend to get stressed out or caught up or mindlessly eat when you are at family gatherings.Okay, you know cut yourself a break, know that that’s, probably going to happen, and fill up on the lower-calorie foods.The carrot sticks the broccoli, the white meat, turkey, anything that’s available, that’s, not like sweet potato pie or brownies, keep water or low-calorie beverage. In your hand, if you’ve got your hand full, you can’t eat at the same time.So you know if you walk around with a cup in your hand, it helps talk to people.Hopefully, you don’t talk with your mouth open or talk with food in your mouth.So if you’re talking to people, you’re not going to be as inclined to go and get something to eat because you’re wanting to stay engaged in that conversation.Stay away from the buffet, especially if you know that it could get stressful, or maybe you know for me, I turn into a pumpkin at like 7 30 at night.I get up at 4 00, but I turn into a pumpkin at 7, 30 and a lot of times holiday parties and those sorts of things are at eight, nine, o’clock at night, and you know I’ve already turned into a pumpkin.So I know that if I go to those I’m going to be more likely to eat just to kind of stay away because I’m tired and it’s a bad habit.It’s not because I’m hungry.So I know I need to stay away from the buffet during those times we rehearse refusal skills.If somebody says. Oh, you, I’ve got to try it by two.This figure out how you’re going to address that ahead of time, because there’s generally probably a lot of really good foods, and you may really want to taste some, but sometimes people who emotionally eat know if they start eating.If they start eating high-fat high calorie foods, they’re going to want to eat everything.So if I start with one bite of a brownie, I’m going to want to eat every suit that’s on the table.If they know that, then they may want to choose to not even go down that road at that juncture, encourage people to stay mindful of their distress meter before they go back for another helping and ask themselves, am I hungry? Am I just wanting to taste what’s here and how do I feel about that? Or am I eating just because I don’t want to be here and I’m bored and I want to fill the time? Have people keep an index card with their coping mantra and two reasons they don’t want to emotionally eat, so I need to be here.I can do this whatever the mantra is that’s going to get them through the night, whatever they’re.Telling themselves that it’s going to help them plow through and make the right choices, but also two reasons that they don’t want to eat, or they’re going to get around it.Maybe they’ve got something at home that they can eat when they get home eating before they go to.The party may also help prevent some grazing holidays, bringing out a lot of emotions in people.Some people struggle with depression, anxiety, jealousy, grief, and anger. You know the whole gamut during this time and during this time there’s food everywhere I mean starting at Halloween when your kids bring home the Halloween candy, which usually lasts about a week in our house baby.Oh, Halloween candy followed by getting ready for Thanksgiving, followed by doing all the baking or whatever you do, and the holiday parties coming up on the December holiday season.There’s just food everywhere, so it’s really easy to cope.If you will, with stress being overwhelmed with being tired by not eating enough healthy food by binging on unhealthy and soothing food if you will so it’s, encouraged it’s important to encourage people to stay.Mindful of why they’re eating what they’re eating, when constantly bombarded with high-fat high carbohydrate foods, people are tempted to eat to feel calm yeah.I challenge anybody to say that they’ve never eaten and go okay.You know I’m.Just focused on this right now I’m not thinking about everything out here and it feels good um.I’m good now, good, probably not the word I should use, but it does help people distract themselves sometimes when they eat, especially those high-intensity foods.You feel happier serotonins are released. Dopamine is released.You’re, like oh, that’s good.I want to do that again or you just feel numb.You can get into a zone where you’re just eating and not caring about it’s.Not that you’re feeling calm, you’re just not feeling anything, and a lot of times when people get into that zone.They’re not tasting the food either.They’re just kind of on autopilot for emotional eating, like most other escape behaviors.Never addresses the underlying emotions and their causes, so we need to look at them.Are you feeling anxious? Are you feeling jittery? Are you feeling depressed because your blood Sugar’s low, because you’re nutritionally deficient because you’re not getting enough sleep or because there’s something cognitive going on, or all of the above emotional eating, often results in physical issues like weight gain Poor sleep and reduced energy weight gain, are you know in and of itself a few pounds here and they’re not a big deal, but some people can start emotionally eating to feel better.They gained a lot of weight. Then they start feeling less energetic.It starts being harder to move around.They get to the point where they are clinically obese.Then they’re going.I’m never going to take all this weight off.They feel hopeless and helpless.You see where this is going, so they eat some more.Can cause poor sleep apnea, it’s hard to get it’s also hard to get comfortable.Sometimes, if you’ve eaten a whole bunch of food right before you go to bed, you know your bellies are all full, and little you wake up.The next morning and your belly are still awful, which means you probably didn’t, sleep very well the night before and emotional eating often results in reduced energy because the foods we binge on the foods we eat for self-soothing often end up causing a sugar Crash some people try to undo emotional eating by restricting other calories which can lead to nutritional deficits and more cravings. I had a girlfriend when I was in high school and you know think back to I don’t know if they still do it, but when we were in high school there was always some kind of candy sale going on and she would always forgo all Other food, so she could have two chocolate bars each day and you know we’re not going to get into the all the other issues surrounding only eating two chocolate bars.But the point I’m making it right now is the fact she wasn’t getting protein.She wasn’t getting it.You know most of her vitamins and minerals and stuff that her body needed to make the neurotransmitter.So she could feel happy and she was contributing to a sugar crash, but I also know that it’s common around the holidays for people to do this.They’ll let go all day without eating because they know they’re going to a party tonight and there’s going to be a lot of really good food doing that once in a while.Not a big deal doing that 10 or 15 times in a month could start to have problems.Emotional eaters need to first find a way to stop before they eat, so, whether it’s writing in a journal or adding.There are a lot of apps on your phone that you can put your food in, even if you’re, not writing about your emotions and your cravings and all that kind of stuff.Sometimes it’s enough to make people stop before they reach. For the food – or you know, kind of an extreme way to go is to not keep pre-processed or prepackaged foods in the house.So anything that you’re going to eat you’ve got to make second identify the underlying reason for your eating figure out.Do I generally eat in response to and then address the thoughts and emotions leading to the urges?So if you figure out the underlying emotions for your eating or your depression, then what thoughts are maintaining that depression? And how can you address it once you address the underlying issues, some of the emotional eating will go away, but some of its habits?We’re going to have to break that habit and, throughout you know, the past couple of decades of working with people.My experience has been the majority of the time people don’t want to hear.Well, once you deal with your emotional issues, the emotional eating will go away now.They’re there because they want to stop that behavior right now.So, yes, we need to work on all the underlying issues but give them a tip or a trick or a tool whatever you want to call it to use before they walk out of your office after every single session.That way, they have something else they can put in their toolbox and feel more empowered to have control over what’s going on with them. And what’s coming their way, having the knowledge of what and why is 80 of helping them get to the recovery point now, if there’s co-occurring or if the eating issues are more than just emotional eating, if there’s, the person meets The criteria for binge eating disorder, bulimia or anorexia.There are a lot of other underlying issues they’re going to have to be dealt with.So I don’t want to trivialize that, but I do want people to feel like they’ve got some hope over what’s going on.Are there any questions? If you enjoy this podcast, please like and subscribe either in your podcast player or on YouTube, you can attend and participate in our live webinars with doctor Snipes by subscribing at all CEUs comm slash counselor toolbox.This episode has been brought to you in part by all CEUs com providing 24 7 multimedia, continuing education, and pre-certification; training to counselors therapists, and nurses, since 2006 use coupon code consular toolbox to get a 20 discount off your order.This month,
If you will, I don’t keep them in the house, but I will allow myself occasionally to buy a small snack-size pack of M Ms, when I’m out or I will get a regular-size pack and I’ll share it with my daughter, so I’m not restricting it.I’m not saying I can never M. Ms again, I’m just not making it available to myself when I might have some unrestricted time, try to avoid buying a bunch of comfort foods and keeping them around the house, and when you’ve got kids when you’ve got family, it’s not entirely possible, usually to not have some of that stuff around but try to avoid having the things that you particularly used for comfort, because if it’s not readily available, then you’ve got to focus on guess what dealing with the emotions.Instead of stuffing them with food, try not to go too long without eating.Like I said earlier, if you go too long, then by the time you get to the food, your blood, Sugar,’s low and you’re just shoveling it as fast as you can initially distract.If you know that you’re getting you’re eating and you’re, like I’m – really not hungry, but I want to eat, take a bath, take a walk, call a friend, heaven forbid get on Facebook.Whatever it is, you can do to distract yourself for 10 or 15 minutes if, after 10 or 15 minutes, you’re still going, I want whatever it is, then you can decide what to do about it.Then, most of the time when people stop and go, I’m not hungry.Let me distract myself.They get caught up in that distraction and before they know it, they’ve forgotten about the craving, and identify the emotions.If you know that you’re not hungry, but you want to eat, then say: okay, what’s going on what’s going on with me? It doesn’t mean that the person is never going to eat when, when they’re upset, because a lot of people do, and is it the end of the world, probably not necessary if they can start reducing the frequency of times that they eat.In response to emotional distress that’s, what we want, we want to progress, not perfect if it’s, depression, what’s causing them to feel hopeless or helpless right now, if it’s, stress, anxiety, or anger, remember our big kind of lump together stuff. What are they stressing out about? Do they feel like they’re overwhelmed? Are they afraid of failure, rejection, and loss of control of the unknown? We’ve gone through those things.We want them to identify what’s going on with them, and then they can make better choices about how to deal with it.So general coping helps them develop, alternate ways of coping with distress.Distract we’ve, already kind of gone over that one.I encourage people – and you know it’s – one of those DBT things – that a lot of therapists encourage their clients to keep a list of things.They can do to distract themselves because it’s not always practical to get up and go on a walk.If you’re at work or it’s, you know two in the morning.So what else can you do to distract yourself? Talk it out with a friend with yourself with your dog? Sometimes you just got to get it out.People who are more auditory will prefer talking it out as opposed to journaling it now.If they talk it out with themselves, they can record it if they want to, or sometimes it’s just better to have a dialogue with themself. If it worked for Freud, it can work for other people journaling.If your clients are inclined to journal, encourage them to write it down.Sometimes just getting stuff out of your head and onto paper will help the feelings dissipate a little bit.So you’re not mulling them over and obsessing over them and getting stuck in those thoughts and feelings.Additionally, while you’re distracted talking it out or journaling, this is also your break.Your stop between the urge and the behavior make a pro and con list of the de-stress, not the eating whatever it is, that’s stressing you out and how can you fix it or what are the pros of this situation and what are the downsides To this situation, encourage them to focus on the positive.You know.If something stressing you out at work, you know you’ve got a big meeting coming up or something you don’t want to do or what it is.You can get stuck on focusing on that or you can focus on the positive that you do have a job.That meeting only comes around once a month. You can it’s time you don’t have to be doing paperwork whatever the pros are for that person encourage them to focus on the positive.If you’re distressed because of some kind of a failure or perceived failure, figure out what you learned from it, whether it was a relationship failure, or maybe you learned what not to do in a relationship anymore. Maybe you learned things that you may have ignored.Maybe you learned what you should have done instead, but how can it be a learning opportunity, instead of somewhere to stay stuck and finally, if something’s making you upset if something’s causing anxiety, depression, hopelessness, helplessness, whatever the negative feeling figure out.If it’s worth your energy to get stuck here, is it worth the turmoil? Is it worth you know having to pacify yourself with food or whatever? It is a lot of times people say you know what now it’s, just it’s, not even worth my effort.It’s not worth moving me away from my goals, because my goal is to stop emotional eating.My goal is to eat for hunger, so I can go to dinner with people and feel comfortable.I can be at a party where there’s a buffet and not feel stressed out that I’m going to go and eat half the stuff on the buffet that’s my goal so is holding on to whatever this de-stress is getting me Closer to being able to do those things and generally the answer:’s no develop alternate ways of coping with the stress the ABCs, the a is the activating event.What is stressing you out and what’s causing the de-stress C is the emotional reaction.Angry depressed stressed, whatever be: are your behaviors? What behaviors or B are your beliefs? Sorry, what are the beliefs that are in there that may need to be addressed? What kind of things are you telling yourself, and, and how can you counter them? Cognitively eliminate your vulnerabilities.You knew we couldn’t get through a presentation without talking about vulnerabilities. If someone is well-rested.Well, the fed has a good social support network, not stretch timewise.Then it will be easier to deal with stress or stressors when they come your way.You’ll have more energy to deal with it, so there won’t be this overwhelming feeling of I just want to bury my head in a jar of peanut butter, be compassionate with yourself.Some days, you know you’re, just going to feel anxious.You’re going to feel depressed.You’re going to get angry.You can beat yourself up over it and you know a lot of people do.Is that the best use of your energy or can you be compassionate? Can you learn from it? Can you give yourself a break and go? You know what I’m having a bad day today and that’s okay, I’m not going to unpack and stay here, but I’m not going to fight.It either helps clients learn how to urge surf help. They understand that, just like a panic attack just like a wave just like a lot of other things in life, it will come, it will crest and it will go out again, so they can sort of identify where they are on the energy of that Urge other tools people can use close the kitchen once I have the kitchen cleaned and you know all the dishes are done and it looks pretty.I hate going in there and finding dishes in the sink again now I’ve got teenagers, so we always have dishes in the sink.But before I had children, you know at seven o’clock.I finished all the dishes and closed the kitchen, and that would be enough motivation for me to not go in there and at least not use plates and stuff to eat.So if we’re saying that we’re going to only eat using utensils plates and sitting and all that stuff that we already talked about, then once you close the kitchen, you’re not going back in, there turn off the light.That also helps so you’re not being attracted to the pretty lights, and you know all the goodies that are in the kitchen to brush your teeth.This is something my grandmother used to do and it works.There’s some research behind it.Minty flavors reduce our appetite.So if you brush your teeth, you get all the other flavors out of your mouth and it reduces your urges to eat because it again it’s clean and fresh. And do you really want to brush your teeth again, and meditate, sometimes just getting in a space where you’re, not obsessing about anything, can help people get past that urge to self-soothe by eating a CT for emotional eating.What am I feeling or thinking about what’s going on with me right now? What is important to me? So if I am thinking I want to eat, I want to you know just dive into this jar of peanut butter, and then I think about what’s important to me.Is it important to me to get control of this? Is it important to me to you know, be able to fit into my clothes in six months or not? So what is it in? What way is controlling my eating habits and eliminating emotional eating important to me, and how does that get me closer to other things that are important to me, and what other things could I do? That would get me closer to my goals.So if the goal is to have improved relationships, be able to feel more comfortable around food reduce the stress around going out to eat, and just around food in general, what else can you do when you are stressed out? Somebody also suggested that adding a blue light in the refrigerator decreases the appeal of foods, which is interesting because yellow red and orange, and browns, I think Pizza Hut – are all foods that increase people’s, hunger and desire to eat.But blue is just a completely different primary color, and adding a blue hue seems like that would be effective, so cool thanks for that.Little tidbit there holiday help, and you know we’re coming into the holidays.So I’ve got to bring that up at every single glass and choose lower-calorie foods.If you tend to get stressed out or caught up or mindlessly eat when you are at family gatherings.Okay, you know cut yourself a break, know that that’s, probably going to happen, and fill up on the lower-calorie foods.The carrot sticks the broccoli, the white meat, turkey, anything that’s available, that’s, not like sweet potato pie or brownies, keep water or low-calorie beverage. In your hand, if you’ve got your hand full, you can’t eat at the same time.So you know if you walk around with a cup in your hand, it helps talk to people.Hopefully, you don’t talk with your mouth open or talk with food in your mouth.So if you’re talking to people, you’re not going to be as inclined to go and get something to eat because you’re wanting to stay engaged in that conversation.Stay away from the buffet, especially if you know that it could get stressful, or maybe you know for me, I turn into a pumpkin at like 7 30 at night.I get up at 4 00, but I turn into a pumpkin at 7, 30 and a lot of times holiday parties and those sorts of things are at eight, nine, o’clock at night, and you know I’ve already turned into a pumpkin.So I know that if I go to those I’m going to be more likely to eat just to kind of stay away because I’m tired and it’s a bad habit.It’s not because I’m hungry.So I know I need to stay away from the buffet during those times we rehearse refusal skills.If somebody says. Oh, you, I’ve got to try it by two.This figure out how you’re going to address that ahead of time, because there’s generally probably a lot of really good foods, and you may really want to taste some, but sometimes people who emotionally eat know if they start eating.If they start eating high-fat high calorie foods, they’re going to want to eat everything.So if I start with one bite of a brownie, I’m going to want to eat every suit that’s on the table.If they know that, then they may want to choose to not even go down that road at that juncture, encourage people to stay mindful of their distress meter before they go back for another helping and ask themselves, am I hungry? Am I just wanting to taste what’s here and how do I feel about that? Or am I eating just because I don’t want to be here and I’m bored and I want to fill the time? Have people keep an index card with their coping mantra and two reasons they don’t want to emotionally eat, so I need to be here.I can do this whatever the mantra is that’s going to get them through the night, whatever they’re.Telling themselves that it’s going to help them plow through and make the right choices, but also two reasons that they don’t want to eat, or they’re going to get around it.Maybe they’ve got something at home that they can eat when they get home eating before they go to.The party may also help prevent some grazing holidays, bringing out a lot of emotions in people.Some people struggle with depression, anxiety, jealousy, grief, and anger. You know the whole gamut during this time and during this time there’s food everywhere I mean starting at Halloween when your kids bring home the Halloween candy, which usually lasts about a week in our house baby.Oh, Halloween candy followed by getting ready for Thanksgiving, followed by doing all the baking or whatever you do, and the holiday parties coming up on the December holiday season.There’s just food everywhere, so it’s really easy to cope.If you will, with stress being overwhelmed with being tired by not eating enough healthy food by binging on unhealthy and soothing food if you will so it’s, encouraged it’s important to encourage people to stay.Mindful of why they’re eating what they’re eating, when constantly bombarded with high-fat high carbohydrate foods, people are tempted to eat to feel calm yeah.I challenge anybody to say that they’ve never eaten and go okay.You know I’m.Just focused on this right now I’m not thinking about everything out here and it feels good um.I’m good now, good, probably not the word I should use, but it does help people distract themselves sometimes when they eat, especially those high-intensity foods.You feel happier serotonins are released. Dopamine is released.You’re, like oh, that’s good.I want to do that again or you just feel numb.You can get into a zone where you’re just eating and not caring about it’s.Not that you’re feeling calm, you’re just not feeling anything, and a lot of times when people get into that zone.They’re not tasting the food either.They’re just kind of on autopilot for emotional eating, like most other escape behaviors.Never addresses the underlying emotions and their causes, so we need to look at them.Are you feeling anxious? Are you feeling jittery? Are you feeling depressed because your blood Sugar’s low, because you’re nutritionally deficient because you’re not getting enough sleep or because there’s something cognitive going on, or all of the above emotional eating, often results in physical issues like weight gain Poor sleep and reduced energy weight gain, are you know in and of itself a few pounds here and they’re not a big deal, but some people can start emotionally eating to feel better.They gained a lot of weight. Then they start feeling less energetic.It starts being harder to move around.They get to the point where they are clinically obese.Then they’re going.I’m never going to take all this weight off.They feel hopeless and helpless.You see where this is going, so they eat some more.Can cause poor sleep apnea, it’s hard to get it’s also hard to get comfortable.Sometimes, if you’ve eaten a whole bunch of food right before you go to bed, you know your bellies are all full, and little you wake up.The next morning and your belly are still awful, which means you probably didn’t, sleep very well the night before and emotional eating often results in reduced energy because the foods we binge on the foods we eat for self-soothing often end up causing a sugar Crash some people try to undo emotional eating by restricting other calories which can lead to nutritional deficits and more cravings. I had a girlfriend when I was in high school and you know think back to I don’t know if they still do it, but when we were in high school there was always some kind of candy sale going on and she would always forgo all Other food, so she could have two chocolate bars each day and you know we’re not going to get into the all the other issues surrounding only eating two chocolate bars.But the point I’m making it right now is the fact she wasn’t getting protein.She wasn’t getting it.You know most of her vitamins and minerals and stuff that her body needed to make the neurotransmitter.So she could feel happy and she was contributing to a sugar crash, but I also know that it’s common around the holidays for people to do this.They’ll let go all day without eating because they know they’re going to a party tonight and there’s going to be a lot of really good food doing that once in a while.Not a big deal doing that 10 or 15 times in a month could start to have problems.Emotional eaters need to first find a way to stop before they eat, so, whether it’s writing in a journal or adding.There are a lot of apps on your phone that you can put your food in, even if you’re, not writing about your emotions and your cravings and all that kind of stuff.Sometimes it’s enough to make people stop before they reach. For the food – or you know, kind of an extreme way to go is to not keep pre-processed or prepackaged foods in the house.So anything that you’re going to eat you’ve got to make second identify the underlying reason for your eating figure out.Do I generally eat in response to and then address the thoughts and emotions leading to the urges?So if you figure out the underlying emotions for your eating or your depression, then what thoughts are maintaining that depression? And how can you address it once you address the underlying issues, some of the emotional eating will go away, but some of its habits?We’re going to have to break that habit and, throughout you know, the past couple of decades of working with people.My experience has been the majority of the time people don’t want to hear.Well, once you deal with your emotional issues, the emotional eating will go away now.They’re there because they want to stop that behavior right now.So, yes, we need to work on all the underlying issues but give them a tip or a trick or a tool whatever you want to call it to use before they walk out of your office after every single session.That way, they have something else they can put in their toolbox and feel more empowered to have control over what’s going on with them. And what’s coming their way, having the knowledge of what and why is 80 of helping them get to the recovery point now, if there’s co-occurring or if the eating issues are more than just emotional eating, if there’s, the person meets The criteria for binge eating disorder, bulimia or anorexia.There are a lot of other underlying issues they’re going to have to be dealt with.So I don’t want to trivialize that, but I do want people to feel like they’ve got some hope over what’s going on.Are there any questions? If you enjoy this podcast, please like and subscribe either in your podcast player or on YouTube, you can attend and participate in our live webinars with doctor Snipes by subscribing at all CEUs comm slash counselor toolbox.This episode has been brought to you in part by all CEUs com providing 24 7 multimedia, continuing education, and pre-certification; training to counselors therapists, and nurses, since 2006 use coupon code consular toolbox to get a 20 discount off your order.This month,




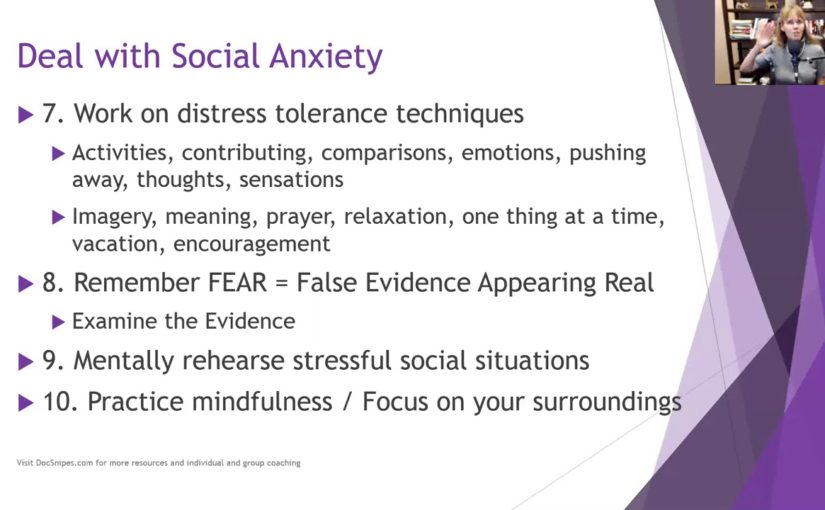


 Etc sometimes you need to
delay joint sessions until the parent or caregiver can offer the child support and sometimes that
means not even starting treatment really until the parent and caregiver parent or caregiver
can be on board now you can get started with psychoeducation emotions identification feelings
identification and stress management and coping skills you know there were not really
poking a bunch of bears so you can probably safely get started on that if it’s sometimes it’s
court-ordered and they have to start treatment by April 1st or something so there are things you can
do but you may need to delay the actual beginning of the trauma narrative until the parent is
able to be available to educate everybody on how therapy works and instill in everyone not just
the parent optima optimist that well optimism about the child’s potential for recovery you
know sometimes they’ve been dealing with this child’s acting out behaviors for so long they’re
just like you know we’ve already been to three other therapists I don’t know what’s going to
fix it or I’ve done everything I know how to do good luck so we can talk about you know a
different approach or we can talk about what they’ve done that’s worked for a short period
of time and build on those strengths to instill optimism and hope and empowerment so
initially, when we talk about psycho-education it’s important to provide accurate information
about the trauma when children are traumatized they can be confused and not completely understand
what happened they may blame themselves and they may hold on to myths because they’ve been misled
and/or deliberately given incorrect information so one of the best ways we can help is to correct
that information provides information about how often this happens and whether you know it’s okay
to do this that or the other psychoeducation clarifies inappropriate information children may
have obtained directly from the perpetrator or on their own so the perpetrator may have told them
that this is how I express love or this is how you need to be disciplined because you don’t learn
this is how I was disciplined whatever it is or they could have gotten it on their own they could
have gotten it from school from the internet or just come up with it in their little heads trying
to make sense of what happened psychoeducation also helps them identify safety issues the
difference between safe situations and dangerous situations and as we get through this I really
want you to get away from the notion that TF CBT and childhood trauma are only physical and sexual
abuse there are so many other traumas as evidenced by the adverse childhood experiences survey that
I want you to wrap your head around that and there are things they didn’t cover in the aces such as
bullying and natural disasters so we want to help children whatever the trauma is the trauma made
they feel unsafe so we want to identify safety issues if the trauma was a hurricane then we want
to talk about what hurricanes are how often they hit what to safety plan etc so every time a
the thunderstorm comes they don’t freak out and we want to use psychoeducation to provide another
way to target faulty or maladaptive beliefs by helping to normalize thoughts and feelings about
the traumatic experience you know it makes sense that that was scary and makes sense that
you’re angry it makes sense that you feel this way and we can talk about why that makes
sense and why it makes you feel that way through cycle education you’re getting the child to start
talking about the specific trauma that he or she experienced in a less anxiety-provoking way by
talking in Jen wrong about the type of trauma so you’re talking about natural disasters you’re
talking about plane crashes you’re talking about domestic violence so they start learning about
it and then eventually you’re going to move down to their experience with it so like I said there
are a ton of different traumas and the ACE study even acknowledges that these are just the ten most
common ones that they heard however there are many many many different traumas and types of trauma
some of the biggest ones are physical and sexual abuse physical neglect emotional abuse
and neglect and the Aces identified mother treated violently I would say anyone in the household
treated violently it’s not just the mother’s substance misuse within the household and that
can be by the parents or by siblings household mental illness parental separation or divorce and
an incarcerated household member so those were aces but then like I said there’s also bullying
the death of a parent or sibling is extremely traumatic hurricane tornado natural disaster and
then I put the fire out separately because sometimes fire can be man-made sometimes it can be a wiring
problem but sometimes it can be Jr was playing with matches now even if jr. Accidentally started
the fire does that make it any less traumatic no it probably makes it more traumatic because then
there’s a whole sense of guilt and responsibility but it’s still a trauma that has to be dealt
with so I put a link to the adverse childhood experiences website if you want to go look more
about that but we’re going to move on psycho-education involves specific information about
the traumatic events the child has experienced not the child’s event we’re not going to go
into police records or something, we’re just going to talk about specific information about
domestic violence or whatever body awareness and sex education in cases of physical or sexual
maltreatment and there are caveats for getting parental consent and permission and all that other
stuff and Risk Reduction skills to decrease the risk of future traumatization now going back to
those other things it’s not just about physical or sexual abuse so we want to look at what was the
the risk created by you know how can you reduce your risk of being bullied how can you reduce your
risk of being traumatized in a tornado you know you can’t stop the tornado from coming
and they’re everywhere so what do you do and talk about a safety plan the same thing with fire
information needs to be tailored to fit a child’s particularly particular experiences and level
of knowledge obviously, you’re going to provide different information to a seven-year-old than
you are to a 17-year-old provide caregivers with handout materials to reinforce the information
discussed in session so this may help educate the parents about some of it but it lets them
know what you talked about and it gets us all on the literal same page you’re providing them a
handout of everything you went over with Junior and we want to encourage caregivers to discuss
this information at home reinforces accurate information about how safe or unsafe they
are and obviously, we’re going towards safe and reinforced accurate information and develop
a safety plan so they feel confident that at home they’re going to be taken care of when you
start psychoeducation you do want to get a sense of what the child already knows and you can use
a question-and-answer game format in which the child gets points for answering questions which I
love this suggestion so you can ask them if you know what is a hurricane or is a tornado and see
if they know and see if they know how much time and much-advanced warning we have for a tornado
versus a hurricane or you know whatever situation you’re talking about you see I did a lot of posts
Hurricane Katrina counseling in northern Florida so that’s one of those things that comes up for
I am talking with children about how likely is it that a category 5 hurricane is going to hit
again but encouraging them to give your aunt’s give answers and if they give the wrong answer you
know it’s great to try now you know try to coach them into a correct answer or provide them the correct
one but give them credit for at least making an effort sample questions might include what is
you know and put in the type of trauma what is bullying how often do you think bullying happens
and why does bullying happen you know those are some questions you can ask to just open a dialogue
about bullying, if this child has been a victim of bullying and is and is traumatized so cultural
considerations meet the child and family where they are by presenting information in a way which
they can relate it to their belief system and you may need to consult with their spiritual
guidance guides leaders whether it be a pastor or you know whatever to get some guidance
on how to handle certain aspects of whether it was the will of God and in the case of sexual abuse
how to handle the concept of virginity and how to handle the concept of bad things happening to bad
people and whatever else they think is coming from or their parents are instilling in them in a
belief system we want to make sure that we’re not necessarily contradicting it and going oh mom dad
and the church is wrong but we also want to help them try to integrate this in a way that can help
they have strong self-esteem so reaching out to those spiritual leaders and the family asking what
their belief system about certain things can be very helpful assess the general beliefs about
the trauma if something happened or when something happens ask the parent or the family that’s there
not necessarily the child but you want to get a sense of what the family stance is on why this
happened what it means how it’s going to impact life hence foreign henceforth and forever more
focus on the events they perceive as traumatic to the family but most especially the child if the
child’s going back to the Aces you know maybe the parents got divorced but the child doesn’t
see that as traumatic because there was domestic violence ahead of time the domestic violence was
traumatic the divorce was a relief so wherever the child is with each trauma we want to
be respectful of what they perceive is traumatic and tailor the information so the family can be
more receptive to it as supportive as possible and sometimes you need to make sure that the language
you know make sure the language is not jargony about general views of mental health and mental health
treatment should also be assessed and addressed in the psychoeducation piece not only with the child
but also with the family, if they are suspicious of it don’t understand it think that you’re just
going to magically fix Junior we want to demystify the process and talk about what is the purpose of
the assessment what is the purpose of each one of these activities and why am I doing this or why
are we doing this as a team and how can it help and then we also want to provide information to
D stigmatize and normalize mental health issues and seeking treatment some cultures are still
resistant to seeking treatment and I use the term cultures broadly because there’s
a stigma associated with it so normalizing for them how many people go to treatment how common
PTSD is or whatever the situation you’re dealing with it doesn’t mean they have to like it but at
At least it will give them a little bit of a nugget to understand that they’re not the only ones if
they are from a cultural group a minority cultural group of some sort you might want to provide
information about how common this particular issue is in their group I’ve done a lot of work
with law enforcement and emergency responders and they’re kind of their little group so
we talk about how common depression is among law enforcement and emergent emergency responders
specifically, because they face so much so many different stressors than you know Joe Schmo over
here so it D stigmatizes and normalizes a little bit now they still may not talk about it and
go well hey you know 37% of us have clinical depression no that’s probably not going to happen
but at least in the back of their mind, they can go you know what I’m looking around this room and
I can bet that at least one other person’s on antidepressants or something and feel a little
less unique and isolated in parent sessions you want to provide a rationale and overview of the
treatment model educates parents about the trauma and talks about the child’s trauma-related symptoms
so we’re going to go over what is hyper-vigilance what is the function it why people become
hypervigilant after trauma and what might it look like in a child because it presents very
differently for different children so we might want to give some ideas and say does this sound
like Johnny or does this sound like Johnny and help them understand why these behaviors may
be coming out we want to talk about how early treatment helps prevent long-term problems okay
maybe the trauma happened three years ago but still, it’s better than waiting ten more years and
you know Johnny’s still not having any Ellucian will want to talk about the importance of talking
directly about the trauma to help the children cope with their experiences and not hedging and
this will be on a case-by-case basis but the manual walks you through handling this discussion with
the parents about exactly how much detail do I go into if Johnny brings it up at home reassure
parents that children will first be taught skills to help them cope with their discomfort
and that talking about the trauma will be done slowly with a great deal of support so we’re not
just going to plop them down and go okay and tell me about the day that all this happened which
is what the child has experienced already if it was reported to law enforcement and/or the child
welfare they’ve probably had somebody sit down and say get right to the nitty-gritty at least
once or twice and it’s completely dehumanizing so we want to reassure parents that we’re not
going to do that to the child again will help the caregiver understand their role in the child’s
treatment since this modified since this model emphasizes working together as a team so I’m not
just going to be educating you it’s not going to be a parallel thing where I go in and I work with
Johnny and then I tell you what I did and then I work with Johnny I’m going to work with Johnny
and then we’re going to discuss what Johnny and I did in session and I’m going to get input from
you and we’re going to talk about how you feel about it and then I’m going to provide you with tools
so you can help Johnny outside of the session because you’re going to be with them for six-and-a-half
other days that I’m not and this can’t work if it’s just one hour once a week and we want to
elicit parent input questions and suggestions as much as possible because they’ve been living with
their kid for you know however many years so they probably have an idea about what works and what
doesn’t so we’ll start with both parents and children in their respective sessions helping
them understand what control breathing is and how it helps slow the heart rate and trigger the
wrist and digest sort of reaction in your body when your breathing slows your heart naturally
slows because the stress reaction tells your brain you’ve got to breathe fast and the heart
rates got to go fast well when you override that then you’re kind of overriding the whole system
and we’ll also talk about thought stopping and this is especially helpful if the trauma is recent
or and/or ever-present in the mind of the youth so they can say I am NOT going to talk about that right
now I’m not going to think about that right talk about distraction techniques go back to
your DBT stuff talks about improving the moment and accepts to help the child develop skills to
handle and work through when those thoughts pop up replace unthawed unwanted thoughts with
a pleasant one so talk about it in session when thoughts like that come up what would you
prefer to think about and then really get into the Nitty Gritty the five senses what do you see
smell hear taste you know help me get into that situation or that thought this teaches that
thoughts even unexpected and intrusive ones can be controlled so that gives them hope and again we’re
not exacerbating the thoughts right now we’re not bringing up their particular trauma and
having them get into detail we are just helping them deal with what’s happening normally on a
day-to-day basis so they feel like they have more control for the older kids you can have them
people log about when this technique is used what they were thinking about and how effective the
thought stopping was and then review it and help them tune it up if it’s not really effective and
give them praise for when they use it effectively relaxation training persons of Asian or Hispanic
origin tend to express stress in more somatic or physical terms so just be aware of that but that
doesn’t mean that Caucasians don’t relaxation training is good for anyone and the medical
school of South Carolina training recommended that relaxation is stress-free and
workbook by Davis Schulman and McKay so and it is still in publication when deciding how to
present relaxation techniques are creative have the child help you to integrate the elements
into the technique that makes it more relevant to them so, what are you thinking about when you
relax you know I know I like to go to the woods but maybe this kid likes to think about a video
game or play with their dog whatever it is but helps them make it relevant to them and then have
they identify other things they do to relax like drawing listening to music walking and making a
list of those things so they can refer to it when you’re teaching relaxation training especially if
you’re doing something like progressive muscular relaxation be sensitive to the child’s wishes if
they don’t wish to close their eyes or lie down which could trigger memories of the trauma we’re
not going there yet so if they feel vulnerable lying down or taking orders like that because
you can imagine how being told to lie down and close their eyes might be a trigger for certain
abuse survivors you know be cognizant of that and say you know get into a comfortable position
or how where would you like to sit while we talk about this like I said parents can often
benefit from the relaxation training as well so because they’re dealing with their issues
about the trauma but they’re also dealing with trying to figure out how to help Johnny and any
of them deal with any of Johnny’s misbehaviors or problematic behaviors then they move on to
feelings identification so it helps the therapist judge the child’s ability to articulate feelings
if you can tell me what makes you happy that’s great but if you can’t then you know we need to
work on figuring out what makes you happy you also want to help the child rate the intensity
of the emotion don’t let them stick with happy mad sad glad and afraid you know let’s talk about
different emotions and use the emotion chart with little faces on it or you can use the emotion
thermometer so is it a hot emotion or is it a cool emotion and helps the child
learn how to express feelings appropriately in different situations I mean sometimes they’re
going to be angry but it might not be appropriate to you know get up and stomp out of the room or
whatever however they communicate it so help them figure out how to articulate that so they can be
heard and supported some children have difficulty discussing or identifying their feelings so
you might try stepping back and discussing the feelings of other children or characters from
books or stories so you know think about Puff the Magic Dragon if they’ve read that you know
that dates me a little bit there but you know how did the little boy feel and talking about things
different characters and different stories where there are elements of anger and shame and loss and
all of that stuff helps children identify how they experience emotions if they seem detached
from the experience because sometimes they just they’ve shut it off it was just too overwhelming
so we want to talk about you know when you’re happy what does that feel like or when you’re
angry what happens what does your body feel like when you’re angry and they might be able
to tell you they hear their heartbeat in their ears or everything gets all fuzzy or whatever
but help them start tuning in to how they react and connecting that with an emotional word and then
after all, that’s done they can identify feelings they can identify feeling intensity now we want to
differentiate between thoughts and feelings many children describe thoughts when they’ve been
asked about a feeling so if you ask them how they feel they may say I want to run away so
you want to say okay well I hear that you want to run away so I’m wondering if you are bored and you
you’re bored and want to get away from it or if you’re scared can you tell me a little bit more
about what it means to you to want to run away during feelings identification the parent
sessions normalize what is going on with their child and help the parent understand that some
children may be seemingly in constant distress or detached from the trauma and that’s okay
we all react differently to traumas so again we’re going to share with the parents what we’re
Do let them know any specific difficulties if any juniors have encouraged the parent to praise
the child for appropriate management of difficult motions and I put in parenthesis successive
approximations because they’re not going to get it a hundred percent right every time so if they
try to effectively manage their emotions even a little bit let’s give them praise for that and
then help them figure out how to do it a little bit better the next time so instead of having a
complete meltdown maybe they got up and stomped out of the room well that’s an improvement so
then we want to talk about how to shape that behavior so it’s a more appropriate communication
if parents have difficulty identifying their own emotions provide them with examples so
continually ask them questions about how you feel when it’s a rainy day outside and how to do you
feel when somebody’s supposed to call you and they don’t how do you feel when and have about 15 or 20
examples and you can have them on a piece of paper and even give it to the parent to take home for
their homework if parents are overcome with their own emotions about the trauma validate
their feelings and explain how children need to see that their parents can handle talking
about the trauma so there the children need to see the strength and the parents which is what you’re
going to work on in parent sessions to make sure that the parents have the resolve and the skills
handle talking about this topic with junior TFC BT can be an effective intervention
for children or adolescents whose primary presenting issue is trauma-related emotional or
behavioral dysregulation TF CBT is not appropriate for clients who are actively suicidal and severely
depressed or currently abusing substances we want to make sure they’re clean
and sober as much as possible TF CBT starts with psychoeducation and then teaches stress
management and coping skills to aid in the management of distressing feelings psycho IDI
helps to clarify the inappropriate information children may have and start getting them a little
a bit more comfortable talking about the topic in general before we start going deeper and
feelings identification helps participants start effectively labeling and communicating their
feelings so they can receive the support and nurturance they need from their caregivers
and their support system if you enjoy this podcast please like and subscribe either in your
podcast player or on YouTube you can attend and participate in our live webinars with dr. Snipes
by subscribing to all CEUs comm slash counselor toolbox this episode has been brought to you in
part by all CEUs calm providing 24/7 multimedia continuing education and pre-certification
training to counselors therapists and nurses since 2006 use coupon code consular toolbox to
get a 20% discount on your order this month.
Etc sometimes you need to
delay joint sessions until the parent or caregiver can offer the child support and sometimes that
means not even starting treatment really until the parent and caregiver parent or caregiver
can be on board now you can get started with psychoeducation emotions identification feelings
identification and stress management and coping skills you know there were not really
poking a bunch of bears so you can probably safely get started on that if it’s sometimes it’s
court-ordered and they have to start treatment by April 1st or something so there are things you can
do but you may need to delay the actual beginning of the trauma narrative until the parent is
able to be available to educate everybody on how therapy works and instill in everyone not just
the parent optima optimist that well optimism about the child’s potential for recovery you
know sometimes they’ve been dealing with this child’s acting out behaviors for so long they’re
just like you know we’ve already been to three other therapists I don’t know what’s going to
fix it or I’ve done everything I know how to do good luck so we can talk about you know a
different approach or we can talk about what they’ve done that’s worked for a short period
of time and build on those strengths to instill optimism and hope and empowerment so
initially, when we talk about psycho-education it’s important to provide accurate information
about the trauma when children are traumatized they can be confused and not completely understand
what happened they may blame themselves and they may hold on to myths because they’ve been misled
and/or deliberately given incorrect information so one of the best ways we can help is to correct
that information provides information about how often this happens and whether you know it’s okay
to do this that or the other psychoeducation clarifies inappropriate information children may
have obtained directly from the perpetrator or on their own so the perpetrator may have told them
that this is how I express love or this is how you need to be disciplined because you don’t learn
this is how I was disciplined whatever it is or they could have gotten it on their own they could
have gotten it from school from the internet or just come up with it in their little heads trying
to make sense of what happened psychoeducation also helps them identify safety issues the
difference between safe situations and dangerous situations and as we get through this I really
want you to get away from the notion that TF CBT and childhood trauma are only physical and sexual
abuse there are so many other traumas as evidenced by the adverse childhood experiences survey that
I want you to wrap your head around that and there are things they didn’t cover in the aces such as
bullying and natural disasters so we want to help children whatever the trauma is the trauma made
they feel unsafe so we want to identify safety issues if the trauma was a hurricane then we want
to talk about what hurricanes are how often they hit what to safety plan etc so every time a
the thunderstorm comes they don’t freak out and we want to use psychoeducation to provide another
way to target faulty or maladaptive beliefs by helping to normalize thoughts and feelings about
the traumatic experience you know it makes sense that that was scary and makes sense that
you’re angry it makes sense that you feel this way and we can talk about why that makes
sense and why it makes you feel that way through cycle education you’re getting the child to start
talking about the specific trauma that he or she experienced in a less anxiety-provoking way by
talking in Jen wrong about the type of trauma so you’re talking about natural disasters you’re
talking about plane crashes you’re talking about domestic violence so they start learning about
it and then eventually you’re going to move down to their experience with it so like I said there
are a ton of different traumas and the ACE study even acknowledges that these are just the ten most
common ones that they heard however there are many many many different traumas and types of trauma
some of the biggest ones are physical and sexual abuse physical neglect emotional abuse
and neglect and the Aces identified mother treated violently I would say anyone in the household
treated violently it’s not just the mother’s substance misuse within the household and that
can be by the parents or by siblings household mental illness parental separation or divorce and
an incarcerated household member so those were aces but then like I said there’s also bullying
the death of a parent or sibling is extremely traumatic hurricane tornado natural disaster and
then I put the fire out separately because sometimes fire can be man-made sometimes it can be a wiring
problem but sometimes it can be Jr was playing with matches now even if jr. Accidentally started
the fire does that make it any less traumatic no it probably makes it more traumatic because then
there’s a whole sense of guilt and responsibility but it’s still a trauma that has to be dealt
with so I put a link to the adverse childhood experiences website if you want to go look more
about that but we’re going to move on psycho-education involves specific information about
the traumatic events the child has experienced not the child’s event we’re not going to go
into police records or something, we’re just going to talk about specific information about
domestic violence or whatever body awareness and sex education in cases of physical or sexual
maltreatment and there are caveats for getting parental consent and permission and all that other
stuff and Risk Reduction skills to decrease the risk of future traumatization now going back to
those other things it’s not just about physical or sexual abuse so we want to look at what was the
the risk created by you know how can you reduce your risk of being bullied how can you reduce your
risk of being traumatized in a tornado you know you can’t stop the tornado from coming
and they’re everywhere so what do you do and talk about a safety plan the same thing with fire
information needs to be tailored to fit a child’s particularly particular experiences and level
of knowledge obviously, you’re going to provide different information to a seven-year-old than
you are to a 17-year-old provide caregivers with handout materials to reinforce the information
discussed in session so this may help educate the parents about some of it but it lets them
know what you talked about and it gets us all on the literal same page you’re providing them a
handout of everything you went over with Junior and we want to encourage caregivers to discuss
this information at home reinforces accurate information about how safe or unsafe they
are and obviously, we’re going towards safe and reinforced accurate information and develop
a safety plan so they feel confident that at home they’re going to be taken care of when you
start psychoeducation you do want to get a sense of what the child already knows and you can use
a question-and-answer game format in which the child gets points for answering questions which I
love this suggestion so you can ask them if you know what is a hurricane or is a tornado and see
if they know and see if they know how much time and much-advanced warning we have for a tornado
versus a hurricane or you know whatever situation you’re talking about you see I did a lot of posts
Hurricane Katrina counseling in northern Florida so that’s one of those things that comes up for
I am talking with children about how likely is it that a category 5 hurricane is going to hit
again but encouraging them to give your aunt’s give answers and if they give the wrong answer you
know it’s great to try now you know try to coach them into a correct answer or provide them the correct
one but give them credit for at least making an effort sample questions might include what is
you know and put in the type of trauma what is bullying how often do you think bullying happens
and why does bullying happen you know those are some questions you can ask to just open a dialogue
about bullying, if this child has been a victim of bullying and is and is traumatized so cultural
considerations meet the child and family where they are by presenting information in a way which
they can relate it to their belief system and you may need to consult with their spiritual
guidance guides leaders whether it be a pastor or you know whatever to get some guidance
on how to handle certain aspects of whether it was the will of God and in the case of sexual abuse
how to handle the concept of virginity and how to handle the concept of bad things happening to bad
people and whatever else they think is coming from or their parents are instilling in them in a
belief system we want to make sure that we’re not necessarily contradicting it and going oh mom dad
and the church is wrong but we also want to help them try to integrate this in a way that can help
they have strong self-esteem so reaching out to those spiritual leaders and the family asking what
their belief system about certain things can be very helpful assess the general beliefs about
the trauma if something happened or when something happens ask the parent or the family that’s there
not necessarily the child but you want to get a sense of what the family stance is on why this
happened what it means how it’s going to impact life hence foreign henceforth and forever more
focus on the events they perceive as traumatic to the family but most especially the child if the
child’s going back to the Aces you know maybe the parents got divorced but the child doesn’t
see that as traumatic because there was domestic violence ahead of time the domestic violence was
traumatic the divorce was a relief so wherever the child is with each trauma we want to
be respectful of what they perceive is traumatic and tailor the information so the family can be
more receptive to it as supportive as possible and sometimes you need to make sure that the language
you know make sure the language is not jargony about general views of mental health and mental health
treatment should also be assessed and addressed in the psychoeducation piece not only with the child
but also with the family, if they are suspicious of it don’t understand it think that you’re just
going to magically fix Junior we want to demystify the process and talk about what is the purpose of
the assessment what is the purpose of each one of these activities and why am I doing this or why
are we doing this as a team and how can it help and then we also want to provide information to
D stigmatize and normalize mental health issues and seeking treatment some cultures are still
resistant to seeking treatment and I use the term cultures broadly because there’s
a stigma associated with it so normalizing for them how many people go to treatment how common
PTSD is or whatever the situation you’re dealing with it doesn’t mean they have to like it but at
At least it will give them a little bit of a nugget to understand that they’re not the only ones if
they are from a cultural group a minority cultural group of some sort you might want to provide
information about how common this particular issue is in their group I’ve done a lot of work
with law enforcement and emergency responders and they’re kind of their little group so
we talk about how common depression is among law enforcement and emergent emergency responders
specifically, because they face so much so many different stressors than you know Joe Schmo over
here so it D stigmatizes and normalizes a little bit now they still may not talk about it and
go well hey you know 37% of us have clinical depression no that’s probably not going to happen
but at least in the back of their mind, they can go you know what I’m looking around this room and
I can bet that at least one other person’s on antidepressants or something and feel a little
less unique and isolated in parent sessions you want to provide a rationale and overview of the
treatment model educates parents about the trauma and talks about the child’s trauma-related symptoms
so we’re going to go over what is hyper-vigilance what is the function it why people become
hypervigilant after trauma and what might it look like in a child because it presents very
differently for different children so we might want to give some ideas and say does this sound
like Johnny or does this sound like Johnny and help them understand why these behaviors may
be coming out we want to talk about how early treatment helps prevent long-term problems okay
maybe the trauma happened three years ago but still, it’s better than waiting ten more years and
you know Johnny’s still not having any Ellucian will want to talk about the importance of talking
directly about the trauma to help the children cope with their experiences and not hedging and
this will be on a case-by-case basis but the manual walks you through handling this discussion with
the parents about exactly how much detail do I go into if Johnny brings it up at home reassure
parents that children will first be taught skills to help them cope with their discomfort
and that talking about the trauma will be done slowly with a great deal of support so we’re not
just going to plop them down and go okay and tell me about the day that all this happened which
is what the child has experienced already if it was reported to law enforcement and/or the child
welfare they’ve probably had somebody sit down and say get right to the nitty-gritty at least
once or twice and it’s completely dehumanizing so we want to reassure parents that we’re not
going to do that to the child again will help the caregiver understand their role in the child’s
treatment since this modified since this model emphasizes working together as a team so I’m not
just going to be educating you it’s not going to be a parallel thing where I go in and I work with
Johnny and then I tell you what I did and then I work with Johnny I’m going to work with Johnny
and then we’re going to discuss what Johnny and I did in session and I’m going to get input from
you and we’re going to talk about how you feel about it and then I’m going to provide you with tools
so you can help Johnny outside of the session because you’re going to be with them for six-and-a-half
other days that I’m not and this can’t work if it’s just one hour once a week and we want to
elicit parent input questions and suggestions as much as possible because they’ve been living with
their kid for you know however many years so they probably have an idea about what works and what
doesn’t so we’ll start with both parents and children in their respective sessions helping
them understand what control breathing is and how it helps slow the heart rate and trigger the
wrist and digest sort of reaction in your body when your breathing slows your heart naturally
slows because the stress reaction tells your brain you’ve got to breathe fast and the heart
rates got to go fast well when you override that then you’re kind of overriding the whole system
and we’ll also talk about thought stopping and this is especially helpful if the trauma is recent
or and/or ever-present in the mind of the youth so they can say I am NOT going to talk about that right
now I’m not going to think about that right talk about distraction techniques go back to
your DBT stuff talks about improving the moment and accepts to help the child develop skills to
handle and work through when those thoughts pop up replace unthawed unwanted thoughts with
a pleasant one so talk about it in session when thoughts like that come up what would you
prefer to think about and then really get into the Nitty Gritty the five senses what do you see
smell hear taste you know help me get into that situation or that thought this teaches that
thoughts even unexpected and intrusive ones can be controlled so that gives them hope and again we’re
not exacerbating the thoughts right now we’re not bringing up their particular trauma and
having them get into detail we are just helping them deal with what’s happening normally on a
day-to-day basis so they feel like they have more control for the older kids you can have them
people log about when this technique is used what they were thinking about and how effective the
thought stopping was and then review it and help them tune it up if it’s not really effective and
give them praise for when they use it effectively relaxation training persons of Asian or Hispanic
origin tend to express stress in more somatic or physical terms so just be aware of that but that
doesn’t mean that Caucasians don’t relaxation training is good for anyone and the medical
school of South Carolina training recommended that relaxation is stress-free and
workbook by Davis Schulman and McKay so and it is still in publication when deciding how to
present relaxation techniques are creative have the child help you to integrate the elements
into the technique that makes it more relevant to them so, what are you thinking about when you
relax you know I know I like to go to the woods but maybe this kid likes to think about a video
game or play with their dog whatever it is but helps them make it relevant to them and then have
they identify other things they do to relax like drawing listening to music walking and making a
list of those things so they can refer to it when you’re teaching relaxation training especially if
you’re doing something like progressive muscular relaxation be sensitive to the child’s wishes if
they don’t wish to close their eyes or lie down which could trigger memories of the trauma we’re
not going there yet so if they feel vulnerable lying down or taking orders like that because
you can imagine how being told to lie down and close their eyes might be a trigger for certain
abuse survivors you know be cognizant of that and say you know get into a comfortable position
or how where would you like to sit while we talk about this like I said parents can often
benefit from the relaxation training as well so because they’re dealing with their issues
about the trauma but they’re also dealing with trying to figure out how to help Johnny and any
of them deal with any of Johnny’s misbehaviors or problematic behaviors then they move on to
feelings identification so it helps the therapist judge the child’s ability to articulate feelings
if you can tell me what makes you happy that’s great but if you can’t then you know we need to
work on figuring out what makes you happy you also want to help the child rate the intensity
of the emotion don’t let them stick with happy mad sad glad and afraid you know let’s talk about
different emotions and use the emotion chart with little faces on it or you can use the emotion
thermometer so is it a hot emotion or is it a cool emotion and helps the child
learn how to express feelings appropriately in different situations I mean sometimes they’re
going to be angry but it might not be appropriate to you know get up and stomp out of the room or
whatever however they communicate it so help them figure out how to articulate that so they can be
heard and supported some children have difficulty discussing or identifying their feelings so
you might try stepping back and discussing the feelings of other children or characters from
books or stories so you know think about Puff the Magic Dragon if they’ve read that you know
that dates me a little bit there but you know how did the little boy feel and talking about things
different characters and different stories where there are elements of anger and shame and loss and
all of that stuff helps children identify how they experience emotions if they seem detached
from the experience because sometimes they just they’ve shut it off it was just too overwhelming
so we want to talk about you know when you’re happy what does that feel like or when you’re
angry what happens what does your body feel like when you’re angry and they might be able
to tell you they hear their heartbeat in their ears or everything gets all fuzzy or whatever
but help them start tuning in to how they react and connecting that with an emotional word and then
after all, that’s done they can identify feelings they can identify feeling intensity now we want to
differentiate between thoughts and feelings many children describe thoughts when they’ve been
asked about a feeling so if you ask them how they feel they may say I want to run away so
you want to say okay well I hear that you want to run away so I’m wondering if you are bored and you
you’re bored and want to get away from it or if you’re scared can you tell me a little bit more
about what it means to you to want to run away during feelings identification the parent
sessions normalize what is going on with their child and help the parent understand that some
children may be seemingly in constant distress or detached from the trauma and that’s okay
we all react differently to traumas so again we’re going to share with the parents what we’re
Do let them know any specific difficulties if any juniors have encouraged the parent to praise
the child for appropriate management of difficult motions and I put in parenthesis successive
approximations because they’re not going to get it a hundred percent right every time so if they
try to effectively manage their emotions even a little bit let’s give them praise for that and
then help them figure out how to do it a little bit better the next time so instead of having a
complete meltdown maybe they got up and stomped out of the room well that’s an improvement so
then we want to talk about how to shape that behavior so it’s a more appropriate communication
if parents have difficulty identifying their own emotions provide them with examples so
continually ask them questions about how you feel when it’s a rainy day outside and how to do you
feel when somebody’s supposed to call you and they don’t how do you feel when and have about 15 or 20
examples and you can have them on a piece of paper and even give it to the parent to take home for
their homework if parents are overcome with their own emotions about the trauma validate
their feelings and explain how children need to see that their parents can handle talking
about the trauma so there the children need to see the strength and the parents which is what you’re
going to work on in parent sessions to make sure that the parents have the resolve and the skills
handle talking about this topic with junior TFC BT can be an effective intervention
for children or adolescents whose primary presenting issue is trauma-related emotional or
behavioral dysregulation TF CBT is not appropriate for clients who are actively suicidal and severely
depressed or currently abusing substances we want to make sure they’re clean
and sober as much as possible TF CBT starts with psychoeducation and then teaches stress
management and coping skills to aid in the management of distressing feelings psycho IDI
helps to clarify the inappropriate information children may have and start getting them a little
a bit more comfortable talking about the topic in general before we start going deeper and
feelings identification helps participants start effectively labeling and communicating their
feelings so they can receive the support and nurturance they need from their caregivers
and their support system if you enjoy this podcast please like and subscribe either in your
podcast player or on YouTube you can attend and participate in our live webinars with dr. Snipes
by subscribing to all CEUs comm slash counselor toolbox this episode has been brought to you in
part by all CEUs calm providing 24/7 multimedia continuing education and pre-certification
training to counselors therapists and nurses since 2006 use coupon code consular toolbox to
get a 20% discount on your order this month.