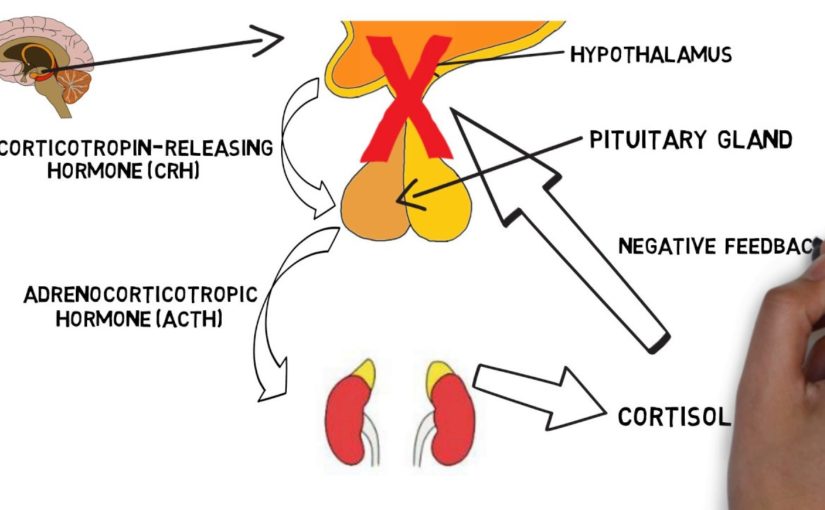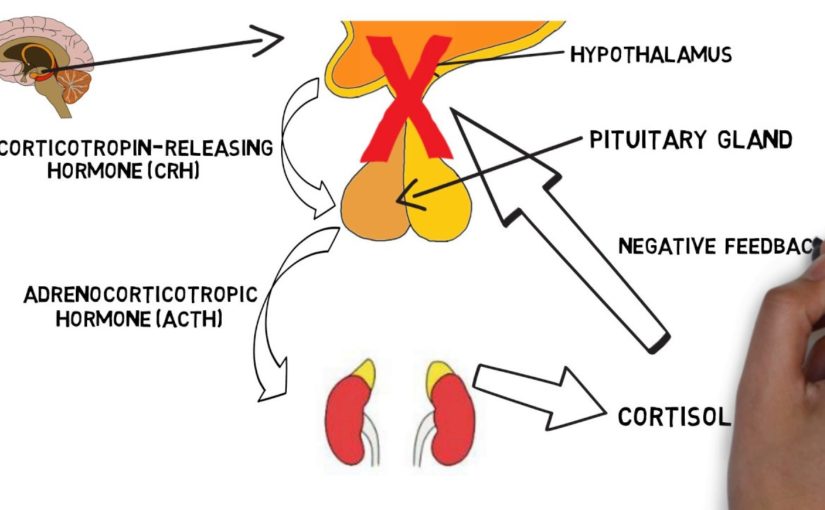
Welcome to Neuroscience for two minutes, where I excuse neuroscience topics in two minutes or Less In this batch, I will explain the HPA axis Both the hypothalamus the pituitary gland the adrenal gland, is known for its axis in its interaction with stress. The HPA axis includes a group of hormonesecreting glands from the nervous and endocrine organizations Under the hypothalamus, pituitary gland and adrenal glands The hypothalamus is the small neural endocrine arrangement set above the ability stanch Authorities the secretion of hormones from the pituitary gland, a hormonal gland Lies merely below the mulch The pituitary can secrete hormones in the bloodstream to reach a variety of purposes In the case of vehicles of the HPA axis, hormones liberated from the pituitary gland are transmitted To the kidneys and alter hormone secretion from the endocrine glands called the adrenal glands Which is located above the kidneys The primary capacity of the HPA axis is to regulate the stress response When we suffer from a traumatic thing, the hypothalamus liberates a hormone called the freeing hormone Corticotropin or( CRH) CRH refers to the pituitary gland to exude a hormone called adrenocorticotropic hormone Or ACTH in the bloodstream ACTH hastens to the adrenal glands where it expects the secrete of a hormone called Cortisol from the adrenal cortex, or outer blanket, from the adrenal glands The secrete of cortisol campaigns a number of changes that help the body cope with stress For lesson: Assists build up energy like glucose, so the body has enough vigor to cope Long press When cortisol degrees rise in the blood This is felt by receptors in the brain regions such as the hypothalamus and the hippocampus, which stops the stress response Through what is known as the mechanism of negative actions Do the rendition: Shwan Hamid Twitter:@ shwanBBBBBhamid

As found on YouTubeNew Explaindio 4 is revolutionary technology which creates fascinating videos by combining 2D & 3D animations, whiteboard sketch elements, and full motion video, all into one powerful, attention grabbing video. This is why I am extremely excited to be able to tell you that now there is Explaindio 4, which is an easy to use video content creation software that allows you to combine 2D & 3D animations, whiteboard sketch elements, and full motion video, all into one powerful, attention grabbing video.

It was the most peaceful, joyous, incredible,
life changing experience I've ever had in my life. There were scary parts, foreboding
parts … I always knew there was beautiful and joy and peace on the other side of it.
It was freeing, it was really freeing. This is Alana. She’s describing what she
felt after she took a dose of this stuff — psilocybin. It’s a naturally occurring psychedelic compound,
the kind you find in magic mushrooms. But she wasn’t tripping in a dorm room or
at Woodstock — it actually wasn’t recreational at all.
If anything became unreal or I was feeling nervous or not in touch with reality, I would
squeeze his hand and he would squeeze mine back just to reassure me that I was okay and
everything was alright. It was part of a controlled medical test to
see if psychedelics could be useful in helping people quit cigarettes. Alana had been smoking
for 37 years before her session with psilocybin, and she hasn’t had a cigarette since. Research on psychedelics for medical use is
preliminary. Most studies suffer from really small sample sizes.
That’s partly because the
federal government lists LSD and psilocybin as Schedule 1 drugs. So researchers face extra
red tape, and funding is really hard to come by. Vox writer German Lopez reviewed dozens of
studies that have been done. He found that psychedelics show promise for treating addiction,
OCD, anxiety, and in some cases, depression. One small study of 15 smokers found that 80
percent were able to abstain from smoking for six months after a psilocybin treatment.
In a pilot study of 12 advanced cancer patients suffering from end-of-life anxiety, participants
who took psilocybin generally showed lower scores on a test of depression.
And smaller study suggested psilocybin treatment could also help people with alcohol dependence
cut back on their drinking days.
We don’t have all the answers as to what
exactly these treatments are doing in the brain. But they seem to work by providing
a meaningful, even mystical experience that leads to lasting changes in a patient's life. The issues that I talked about, or thought about, or went into during my experience were transformative in the sense that I got to look at them through a different lens. I know this sounds weird, I feel like I have more connections in my brain that I couldn't
access before That feeling that Alana is describing is actually
pretty spot-on. When you take LSD your brain looks something
like this. You can actually see a higher degree of connectivity
between various parts of the brain, it’s not limited to the visual cortex.
This communication inside the brain helps explain visual hallucinations — and the researchers argue that it could
also explain why psychedelics can help people overcome serious mental issues.
They wrote that you can think of psychiatric disorders as the brain being “entrenched
in pathology.” Harmful patterns become automated and hard to change, and that’s what can make
things like anxiety, addiction and depression very hard to treat. That’s Albert Garcia-Romeu, he’s a Johns Hopkins researcher who worked on studies of
of psilocybin and smoking addiction, like the one that Alana's involved with. He says that when participants take psychedelics, One of the big remaining questions here is
how long these benefits actually last after just the one-time treatment.
A review of research on LSD-assisted psychotherapy and alcoholism found no statistically significant
benefits after 12 months. And a recent study on psilocybin and depression
found that benefits significantly dropped off after three months. And of course are some big risks to using
psychedelic drugs. It’s hard to predict a patient’s reaction
and some might actually endanger themselves.
Those predisposed to psychotic conditions
are especially at risk for having a traumatic experience while on the drug.
It’s difficult to draw solid conclusions from the existing studies.
But there’s more than enough promise here to merit further research and further funding
for that research. As Matthew Johnson of Johns Hopkins said,
"These are among the most debilitating and costly disorders known to humankind.” For
some people, no existing treatments help. But psychedelics might. One thing you might still be wondering is why so much of this research is so new, when we've known when we've known about psychedelics for thousands of years. Well since these drugs are so old, they can't be patented, which means that pharmaceutical companies don't really have any incentive to fund any research into them.
So that really leaves it up to governments and private contributors to fund all these studies. And there actually was a lot of research done into these drugs in the 50s and 60s, but there was a big enough backlash to the abuse of psychedelics in that period, especially around events like Woodstock, that funding really dried up, and research stopped. And that's why it's only now that we see this research happening, with private, not government contributions..

Translator: Abdul Ameti Reviewer: Helena Bedalli In the mid-90s CDC and Kaiser Permanente discovered an anomaly that dramatically increases risk for seven of the top 10 causes of death in the US. In large doses, it affects brain development, immune and hormonal system and also the way our DNA is read and transcribed. People who are affected by this anomaly in very large doses have three times the risk of death from heart disease, lung cancer, and a 20-year volatility of life expectancy. In addition, doctors are not trained for daily examination and healing. The anomaly I am talking about is not something chemical. It is the trauma of childhood. What trauma are we talking about? I’m not talking about failing the exam, or losing a basketball game.
I'm talking about such harsh and penetrating threats which in the first sense of the word convey to us and change our physiology things like: abuse, negligence or growing up with a parent suffering from a mental illness or drug-dependent. For a long time, I looked at these things the way I was trained to look: or as a social problem – referred to in social services or as a mental health problem – referred to medical services.
Then something happened that made me reconsider my whole approach. When I finished the internship, I wanted to go to a place where I felt needed a place where I could make a difference. And I went to work for the California Pacific Medical Center, one of the best private hospitals in Northern California, and together, we opened a clinic in Bayview-Hunters Point, one of the poorest and neglected neighborhoods in San Francisco. Before we talk about this, was just a pediatrician all over Bayview to serve more than 10,000 children, so we got down to business, and gave great quality of treatment regardless of financial capabilities. It was something so beautiful. We targeted typical health inequalities access to medication, vaccination rates, hospitalization rates for asthma, and broke all records. We felt very proud of ourselves. But then, I started noticing a worrying trend. Many children referred to me for “Concentration Disorders and Hyperactivity ”(ADHD) but in fact, when I did one deep historical and physical research what I found is that many of my patients I could not diagnose them with ADHD.
Many of the children I checked had experienced such severe trauma so much so that I felt something else was happening. Somehow, something important was escaping me. Before I started my internship, I completed my master's degree in public health and one of the things to teach in public health school is that, if you are a doctor and sees 100 children drinking from the same well and 98 have diarrhea you can start and write recipes dose-by-dose antibiotics or go to the place and say, "What the hell is going on in this well?" So I started reading everything that came my way about how exposure to disasters affects a child’s developing mind and body. And one day, my colleague came to my office and said: "Dr. Burke, have you seen that?" In his hand was a copy of a study called "Study of Childhood Disaster Experiences" That day changed my internship at the clinic, and finally my career. Study about childhood disaster experiences it is something that everyone should know. It was done by Dr.
Vince Felitti in Kaiser and Dr. Bob Anda on CDC, and together they interviewed 17,500 adults about their experiences about what they called "child misfortune" (ACE) These included physical, emotional or sexual abuse; physical or emotional neglect; parental mental illness, drug addiction, imprisonment; parental separation or divorce; or domestic violence. For each positive response, they received a point on the ACE score. What did they do then was the correlation of these ACE results against health consequences. What they found was surprising. Two things: Number one: ACEs are more common. 67 percent of the population had at least one ACE, and 12.6 percent, or 1 in 8 had four or more ACEs. The second thing they found was a "dose-response" relationship The higher the ACE score, the more severe the health consequences. For a man with an ACE score of four or more risk of chronic obstructive pulmonary disease was 2 and a half times larger than in a man with an ACE zero score.
For hepatitis, also 2 and a half times larger. For depression, 4 and a half times. For suicide, 12 times. A man with an ACE score of seven or more there was three times more risk to life from lung cancer. and 3 and a half times the risk of ischemic heart disease. the number one killer in the US. Of course that makes sense. Some people saw this data and said, “Look. If you had a difficult childhood, you are more likely to drink alcohol. and to smoke and do all those things that destroy health. This is not science.
It's just bad behavior. " This is exactly where science intervenes. Now we understand better than ever, how early disasters affect the development of the brain and body of children. Affects "nucleus accumbens" (from lat. Supported nucleus) the center of pleasures and rewards in the brain which is involved in drug addiction. It inhibits the parafrontal cortex which is necessary for the control of impulses and executive functions a critical space for learning. In MRI scanners we notice measurable differences in amygdala, fear response center. So there are obvious neurological reasons why people are exposed to large doses of adversity are more likely to exhibit high-risk behaviors, and this is important to know. But it turns out that although they do not exhibit high-risk behaviors, individuals are more likely to develop heart disease or cancer.
The reason has to do with the hypothalamic-pituitary-adrenal axis, which is the brain and body reaction system, who oversees the reaction called “fighting or running”. How does this work? So imagine you are walking in the woods and see a bear. Immediately your hypothalamus sends a signal to your pituitary gland which signals the adrenaline gland that says: "Release the stress hormones! Adrenaline! Cortisol!" And so your heart starts beating, Your eyelashes expand, the airways open, and you are ready to either fight him or run away from the bear. And that's great, if you are in the woods and there is a bear. (Laughter) But the problem is, what happens when the bear comes home every night, and this system is constantly activated and passes from being appropriated, or life-saving at detrimental health pressure.
Children are especially sensitive to repetitive stressful activity because their brain and body is developing. Large doses of disasters not only affect structure and function of the brain but adversely affect the development of the immune system, development of the hormonal system, even the way our DNA is read and transcribed. So for me this information threw out my old training window, because when we understand the mechanism of a disease, when we know not only which roads are interrupted, but like us as doctors, to use science for prevention and recovery.
This is what we do. So in San Francisco, we set up a Youth Welfare Center, for the prevention, examination and treatment of the impact of ACE and toxic stress. We just started with routine examination of each of our children, in their physical activities because I know that if my patient has 4 in the ACE result is 2 and a half times more likely to develop hepatitis or lung disease is 4 and a half times more likely to get depressed, and 12 times more attempted suicide, than my patient with zero ACE. I know this when he (the patient) is in my examination room. For patients with a positive test, we have a very disciplinary team working to reduce disaster doses and treats symptoms using the best ways to include home visits, coordination of care, mental health care, nutrition holistic interventions, and yes, we also give them medication if needed. But we also educate parents about the impact of ACE and toxic stress in the same way that it would take to cover electrical outlets or lead poisoning, and we expand the care of our asthmatics and diabetics in a way that justifies that you may need tougher treatment taking into account hormonal and immune changes.
So the other thing that happens when you understand this science, is desire to shout with fingers in ear because this is not just a child issue in Bayview. I immediately thought that anyone who would find out about this, we would have daily examinations, treatments with multidisciplinary teams and would be a competition for the most effective clinical protocols of healing. But no. This did not happen.
And it was a very good lesson for me. What I thought was just the best medical practice, i understand it to be a whole move. In the words of Dr. Robert Block, former President of the American Academy of Pediatrics, “Childhood Disasters are the only two most unaddressed threats to public health which our nation is facing today. " And for many people this is a terrible prospect. The extent and extent of this problem seems so extensive that it seems futile to think about how we could approach them. But for me, that's where the hope lies, because when we have the right system, when we are clear that this is a public health crisis, then we can start using the right tools to find solutions. From nicotine and lead poisoning to HIV / AIDS The U.S. actually has a strong past in addressing of public health problems, but to repeat these successes with ACE and toxic stress, we will need determination and commitment, and when I see what the reaction of our nation has been so far, I ask myself, "Why haven't we taken this more seriously?" You know, at first I thought we marginalized this issue because it doesn’t apply to us.
This is an issue for those children in those neighborhoods. Which is weird, because the data doesn't prove it. The original ACE study was performed on a population which was 70 percent white race, 70 percent, with high school. But then, the more I talked to people, I began to think that I might have understood it backwards. If I were to ask how many people in this room have grown up with a family member who has suffered from mental illness I bet some of you would raise your hands. And if I were to ask how many people have had one parent who probably drank too much, or who believed that he who loves you beats you I bet some more hands would be raised. Even in this room, this is an issue that affects many of us, and I am beginning to believe that we are marginalizing this issue precisely because it applies to us as well. Maybe it's better to look elsewhere because we don’t want to see it.
We would rather stay sick. Thankfully, scientific achievements, and, to be fair, economic reality makes this option less likely every day and more. The science is clear: Early disasters dramatically affect life expectancy. Today, we are beginning to understand how to stop the transition from early facts in premature death, and 30 years earlier, child with high ACE score, and whose behavioral symptoms are invisible whose asthma management is not related and continuing to develop high blood pressure, and early heart disease or cancer, will be just as abnormal as a 6-month HIV / AIDS mortality. People will look at this situation and say, "What the hell happened there?" This is curable.
That could be. The only thing that matters most is that we need it today the courage to look this problem in the eye and to say that this is true and is for all of us. I believe we are the movement. Thank you. (Applause) .

[♪ INTRO ] If you’ve ever experienced anxiety and depression
— in the clinical sense, I mean — you’ll know that they can feel really different. With anxiety, you’re all ramped up. And with depression, you’re very, very down. Yet they tend to go together. And a lot of medications, especially certain
types of antidepressants, can be used to treat both. We still don’t know a ton about how exactly
anxiety and depression work in the brain — or how antidepressants work to treat them. But over time, psychologists have come to
realize that the two types of conditions are surprisingly similar. They may feel very different in the moment. But they actually have a lot of symptoms in
common, and involve some very similar thought patterns. They might even have similar brain chemistries. So if you’re looking to understand a little
more about how anxiety and depression manifest themselves — whether for yourself or for
someone else in your life — those connections are a good place to start.
Depression and anxiety aren’t really specific
disorders — they’re generic terms for types of disorders. But the most common, and most closely linked,
are major depressive disorder, or MDD, and generalized anxiety disorder, or GAD. In any given year in the U.S., where it’s
easiest to find detailed statistics, about 7% of the population will have MDD, and about
3% will have GAD. Lots of those people have both: About 2/3
of people with major depression also have some kind of anxiety disorder, and about 2/3
of people with generalized anxiety disorder also have major depression. And whether you have one or the other or both,
the same medications are often at the top of the list to help treat it — usually antidepressants. Unsurprisingly, psychologists have noticed
these statistics. But for a long time, we’ve thought of generalized
anxiety and major depression as very different things, and understandably so. Probably the most noticeable symptom of anxiety
is arousal, which in psychology is a technical term rather than a specifically sexual thing. It basically just means being on high alert
— whether psychologically, with increased awareness, or physically, with things like
a racing heart and sweaty palms.
Arousal isn’t part of major depression,
though. And there’s a key symptom of MDD that doesn’t
usually show up in generalized anxiety: low positive affect, which is the technical term
for not getting much pleasure out of life and feeling lethargic and just kind of … blah. So there are important differences between
anxiety and depression, which is part of why they’re still considered separate classes
of disorders. But when you look at the other symptoms, you
start to realize that major depression and generalized anxiety have almost everything
else in common. There’s restlessness, fatigue, irritability,
problems with concentration, sleep disturbances … the list goes on.
And that’s just in the official diagnostic
criteria. So for decades, psychologists have been examining
the models they use to describe anxiety and depression in the brain to see if they point
to a similar source for both types of disorders. They’ve come up with lots of different ideas,
as researchers do, but the most common ones tend to center around the fight or flight
response to stress. Fight or flight kicks in when you’re confronted
with something your mind sees as a threat, and it automatically prepares you to either
fight or run away. And when you think about it, anxiety and depression
are just different types of flight. Psychologists often characterize anxiety as
a sense of helplessness, at its core, and depression as a sense of hopelessness. Anxiety might feel like you’re looking for
ways to fight back. But part of what makes it a disorder is that
it’s not a short-lived feeling that’s easily resolved once you have a plan.
Of course, as with all things mental health,
anxiety disorders can be deeply personal and won’t feel the same for everybody. But clinical anxiety does tend to be more
pervasive. The worry sticks around and starts to take
over your life because it doesn’t feel like something you can conquer. So anxiety and depression might just be slightly
different ways of expressing the same flight response: helplessness or hopelessness. And maybe that’s part of why they so often
go together. That connection also shows up on the biochemical
side of the stress response. There are a lot of hormones involved in this
response, and their effects interact in super complex ways that scientists still don’t
fully understand.
But both depressive and anxiety disorders
are closely associated with an oversensitive stress response system. Researchers think that’s one reason both
of these types of disorders are so much more common in people who’ve experienced major
stresses like trauma or childhood abuse. Those stressors could make their stress response
system more sensitive. The main hormones involved aren’t always
the same, but the changes can cause some of the same symptoms — problems with sleep,
for example. So anxiety and depression seem to be two sides
of a similar reaction to stress, in terms of both thought processes and hormones. Still, that doesn’t really explain why some
antidepressants can treat both anxiety and depression. Because those medications primarily affect
neurotransmitters, the molecules your brain cells use to send messages to each other. If you thought we had a lot left to learn
about how the stress response works, we know even less about what the brain chemistry of
anxiety and depression looks like, or how antidepressants help. But if the thought processes and physical
responses that go along with these disorders aren’t quite as different as they seem on
the surface, it makes sense that the brain chemistry would be similar, too.
And that’s exactly what scientists have
found. More specifically, lots of studies have pointed
to lower levels of the neurotransmitter known as serotonin as a major factor in both anxiety
and depression. Researchers have even identified some more
specific cellular receptors that seem to be involved in both. There’s also some evidence that the way
the brain handles another neurotransmitter, norepinephrine, can be similar in both anxiety
and depression. Since most antidepressants work by increasing
serotonin levels, and some of them also affect norepinephrine, that could explain why they’re
so helpful for both anxiety and depression. Although again, there’s a lot we don’t
know about their exact mechanisms. Ultimately, there’s no denying that in the
moment, anxiety and depression can seem like very different feelings. And if someone has both types of disorders
— well, it’s easy to see how that could feel overwhelming. Like, it’s hard enough treating generalized
anxiety or major depression on their own.
And it’s true that it is often harder to
treat these conditions when someone has both. But maybe not twice as hard. After all, anxiety and depressive disorders
have a lot in common, from their symptoms to the basic brain chemistry behind them to
some of the treatments that can help. The fact that they often go together can be
really tough. But understanding more about why that is has
also pointed us toward better treatments and more effective therapies, that really can
help. Thanks for watching this episode of SciShow
Psych. If you're looking for someone to talk to about
your mental health, we left a few resources in this video’s description. And if you'd like to learn more general info
about treatments, you can watch our episode on misconceptions about antidepressants. [♪ OUTRO ].
Science Documentary: Mental Health Disorders, Brain Trauma, Stress and Anxiety, a Documentary on the BrainDealing with mental health disorders is one of the greatest challenges facing governments around the globe. Diseases such as
alzheimers and depression rob the individual and society of mental capital and well being. One in four people suffer from a mental health disorder. Disorders like alzheimers, schizophrenia, depression, mania, etc. , impact our cognitive functioning. And as a result, it impacts how we function in our homes and at work. So it is imperative to detect these disorders early, and treat them early.There are two types of cognition. There is cold or rational cognition, and hot cognition. Cold cognition helps us make the majority of our decisions in our daily life. Hot cognition helps us with making social decisions and emotional decisions.There are key areas of the brain that respond to stress and trigger anxiety. The thalamus is the area of the brain that responds to sights and sounds. The thalamus breaks down things we see by size, shape and color and then sends a signal to the cerebral cortex. This gives the things we see meaning and enables us to be conscious of what we are seeing or hearing. The prefrontal cortex is very important for stopping the anxiety response after a threat has gone away. The section of the brain that is responsible for emotion is the amygdala. The amygdala’s primary function is to trigger the fear response. The bed nucleus of the striaterminals prepetuates the fear response the locus ceruleus receives a signal from the amygdala and causes rapid heart beat, sweating, pupil dilation and other classic anxiety responses. The hippocampus is the part of the brain that stores memory or emotional baggage derived from stressful situations. Stress, anxiety, and fear are triggered through your senses. Fear is a essential, and very useful, response; whereas anxiety is something that is completely irrational.You think with your brain, and ideas are not floating in air. So how do you get ideas from neurons? Because you think with your brain, every idea you have is physical, and is given by a neural circuit in the brain. Many of those neural circuits are fixed for life, and so are the things you learn early on in life and very often they are metaphorical ideas. So if you do not have a neural circuit for understanding an idea, you wont understand it at all. The classical view of what reason actually is, has failed. And that view says that all reason is conscious, but in fact, 98% is unconscious. This is because the brain functions in parallel and reason, or consciousness, functions linearly. Many things are happening inside your brain and you don’t even truly understand why they are there. People mostly think in frames and metaphors. Metaphors are not in language, but are in thought.Science Documentary: Anti-angiogenesis, Immunotherapy, Vaccines
Science Documentary: Creating Brain Systems,Quantum Computing, Quantum mechanics and Consciousness
Science Documentary: Personalized Medicine, Synthetic Biology , a documentary on genetic design
Science Documentary: Stem Cells,Regenerative Medicine,Artificial Heart,a future medicine documentary
Science Documentary: Cognitive science , a documentary on mind processes, artificial intelligence
Science Documentary: 3D Printing, 3D Imaging, Ultra Fast Laser Imaging Technology
Science Documentary: Flexible Tech, Flexible Wearable Technology, a Documentary on Future Technology
Science Documentary: Artificial Intelligence, Cloud Robots, Trusting Technology
Science Documentary: Augmented Reality, Nanotechnology, Artificial Intelligence
Science Documentary:Future Scenarios, Nanotechnology, Carbon Nanotubes, Nanomagnetism
Alie knows all about how stressful grad school can be. But what happens when stress is more than just stress? This week, we’re talking about the neuroscience of anxiety. And for Alie, it’s personal.Sources:
https://www.adaa.org/understanding-anxiety/generalized-anxiety-disorder-gad
https://www.nimh.nih.gov/health/statistics/prevalence/any-anxiety-disorder-among-adults.shtml
https://www.dartmouth.edu/~rswenson/NeuroSci/figures/Figure_31.htm
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3684250/
http://www.caam.rice.edu/~cox/wrap/norepinephrine.pdf
http://www.mayoclinic.org/diseases-conditions/depression/in-depth/antidepressants/art-20044970Support us on Patreon – https://www.patreon.com/neurotransmissionsHUGE thanks to our Patreon supporters, particularly to Ryan M. Shaver, Carrie McKenzie, and Brandon Cisneros – our Patreon Producers. Thanks you three!Neuro Transmissions is a channel on a mission to bring neuroscience to everyone. It’s not rocket surgery, it’s brain science! Learn all sorts of fun and interesting things with Alie Astrocyte every other Sunday by subscribing to the channel. Have a topic you want covered? Let us know in the comments. Share, like, and subscribe for more videos to come! Over and out.Neuro Transmissions is on the other social medias too:
https://www.facebook.com/neurotransmissions https://www.instagram.com/neurotransmissions
Welcome to Neuro Transmissions
Snapchat – @neuroyoutubeBrain images from Motifolio drawing toolkits (www.motifolio.com)“In The Mist” by Trackmanbeatz is licensed under a Creative Commons Attribution 4.0 International License.
Artist: www.trackmanbeatz.com
“Hoedown” by Audionautix is licensed under a Creative Commons Attribution license (https://creativecommons.org/licenses/by/4.0/)
Artist: http://audionautix.com/The following images and video are Creative Commons and were used for educational purposes:
https://en.wikipedia.org/wiki/National_Institute_of_Mental_Health
https://upload.wikimedia.org/wikipedia/commons/thumb/5/55/GABA_3D_ball.png/1200px-GABA_3D_ball.png
https://upload.wikimedia.org/wikipedia/commons/3/3d/PET-MIPS-anim.gif
https://upload.wikimedia.org/wikipedia/commons/thumb/4/4d/US-NIH-NIMH-Logo.svg/1280px-US-NIH-NIMH-Logo.svg.pngThe following images were used for educational purposes and fall under fair use laws:
https://www.adaa.org/finding-help/treatment/choosing-therapist
https://fanart.tv/fanart/tv/76316/showbackground/mr-bean-57c499f019e81.jpg
https://i.ytimg.com/vi/G8GVWhviw8s/hqdefault.jpg
http://www.hdfinewallpapers.com/HDWallpapers/Big/Miley-Cyrus/Miley_Cyrus_with_Funny_Face_HD_American_Popular_Singer_Wallpaper.jpgClip from This Is Spinal Tap was used for educational, non-profit purposes.All other content is original and/or owned by Neuro Transmissions.
Dr. John J. Medina, a developmental molecular biologist and an affiliate Professor of Bioengineering at the University of Washington School of Medicine, has a lifelong fascination with how the mind reacts to and organizes information. He is the author of the New York Times bestseller “Brain Rules: 12 Principles for Surviving and Thriving at Work, Home, and School” — a provocative book that takes on the way our schools and work environments are designed. Medina’s book on brain development is a must-read for parents and early-childhood educators: “Brain Rules for Baby: How to Raise a Smart and Happy Child from Zero to Five.” His latest book in the series is “Brain Rules for Aging Well: 10 Principles for Staying Vital, Happy, and Sharp.”Dr. Medina joins us in our Google Seattle office to talk about what we all can do for our future selves to Age Well, and why it’s never too early to start. Using clever anecdotes and captivating speaking style, he shares insights on how friendship and the power of reminiscence can have visible and reproducible effects on aging.Get the book here: https://goo.gl/8JHHX4
Brain Health and Nootropics | Podcast #203Thyroid Reset Summit: www.thyroidresetsummit.comGet Show Updates Here: http://www.beyondwellnessradio.com/newsletterYou-tube Podcast Subscribe: http://www.youtube.com/subscription_center?add_user=justinhealthShow Transcription: https://justinhealth.com/brain-health-nootropics-evan-brand-podcast-203/Schedule a FREE Consult: http://www.justinhealth.com/free-consultationMold Problem?
Visit: https://justinhealth.com/immunolyticsOur brain is one of the essential parts of our body — it serves as the coordination center that helps us think, decide, feels, and all the other beautiful functions. In this episode, tune in to Dr. J together with his guest Evan Brand on brain health and nootropics. Learn more about how we improve our brain health and performance, and what is a proper diet for a better brain function.Watch this video for any tips and techniques that may apply to you!In this episode, we cover:00:46 Steps to improve brain performance03:42 Get the gut right16:07 Get the inflammation down18:32 Focus on your diet32:03 Resveratrols and alcohols34:27 Pharmaceutical nootropics=====================================Subscribe on I-Tunes: http://www.beyondwellnessradio.com/itunesReview us at: http://www.beyondwellnessradio.com/itunesVisit us at: http://www.beyondwellnessradio.comHave a question: http://www.beyondwellnessradio.com/question-~-~~-~~~-~~-~-
Please watch: “GI Issues — Malabsorption, Infection & Inflammation in the Eye and Joint | Dr. J Live Q & A”
-~-~~-~~~-~~-~-
Everyone has the ability to build mental strength, but most people don’t know how.
We spend a lot of time talking about physical strength and physical health, but much less time on mental strength and mental health.
We can choose to perform exercises that will help us learn to regulate our thoughts, manage our emotions, and behave productively despite our circumstances – the 3 basic factors of mental strength. No matter what your goals are, building mental strength is the key to reaching your greatest potential.Amy Morin is a licensed clinical social worker and psychotherapist. Since 2002, she has been counseling children, teens, and adults. She also works as an adjunct psychology instructor.
Amy’s expertise in mental strength has attracted international attention. Her bestselling book, 13 Things Mentally Strong People Don’t Do, is being translated into more than 20 languages.
Amy’s advice has been featured by a number of media outlets, including: Time, Fast Company, Good Housekeeping, Business Insider, Elle, Cosmopolitan, Success, Glamour, Oprah.com, TheBlaze TV, and Fox News. She has also been a guest on dozens of radio shows.
She is a regular contributor to Forbes, Inc., and Psychology Today. She serves as About.com’s Parenting Teens Expert and Discipline Expert.
As a frequent keynote speaker, Amy loves to share the latest research on resilience and the best strategies for overcoming adversity and building mental muscle.This talk was given at a TEDx event using the TED conference format but independently organized by a local community. Learn more at http://ted.com/tedx
https://youtube.com/watch?v=3y7AirF3qTs
Episode 1 https://youtu.be/FUDG4h1RqC4
The #Gut-#Brain #Connection: #HowTo #Heal #Your Gut, To Heal Your #Brain
Episode 3 https://youtu.be/23LyPSvsMtg